Respiratory Outpatient Clinic: Update for Providers
Updated August 2021
Due to the COVID-19 pandemic, the Children’s Mercy Respiratory Outpatient Clinics (ROC) will continue to remain closed at all locations.
Although ROC is not available, we are still able to suction patients as needed during both Urgent Care and Emergency Department visits following patient assessment. If you have diagnosed a patient with bronchiolitis, we have telehealth options for triage, Urgent Care appointments and emergency care.
In order to support you and the families you care for, please refer to the additional resources below.
Escalation of care
For patients who need to be seen at Children’s Mercy Urgent Care Centers or the Emergency Department for suctioning, we will focus on providing nasal aspiration rather than nasopharyngeal suctioning, when possible, to reduce the amount of aerosol-generating procedures.
Our Urgent Care locations are available for telehealth as well as in-person visits seven days a week:
- In-person hours: 10 a.m. to 8 p.m. every day
Please encourage families to select a visit time at their preferred location and check in online using Save My Spot to reduce wait time.
Telehealth
Through telehealth visits, families can connect with a provider who can assess their child and help determine if escalation of care is necessary. Historically families have expressed that part of the value of ROC is the ability to see a health care professional who can provide them peace of mind by assessing their loved one, and then offering guidance around escalating care, and/or letting them know their child looks comfortable enough to stay home.
Nurse Advice Line
Families may also contact the Children’s Mercy Nurse Advice Line at (816) 234-3188 where nurses are available 24/7 to answer questions.
In-person Urgent Care visits
If a child needs to be seen, we encourage families to reserve a slot at one of our Urgent Care locations by using Save My Spot. We will provide suctioning in the Urgent Care as needed. In case of an emergency, families should go to one of our Emergency Department locations.
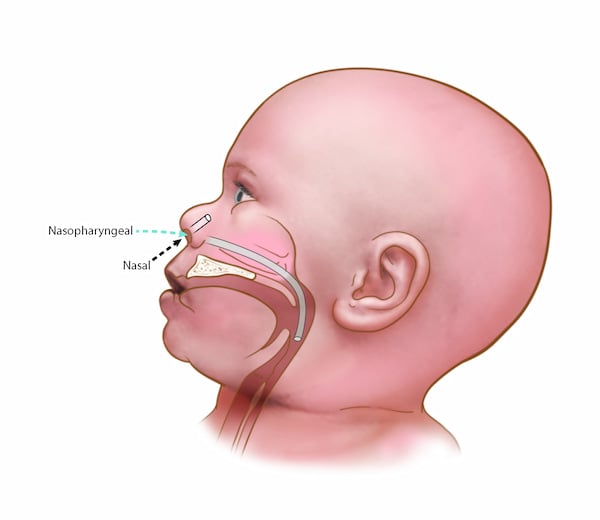
Types of nasal suctioning
Nasal aspiration with a bulb tip
Use a bulb syringe or nasal aspirator attached to oral suction by the parent, or portable or wall suction source to suction mucous from the nose. Put two drops of normal saline (saltwater) in each nostril before suctioning. This may help remove more mucous. Suction before feeding, before sleeping, or if your child appears uncomfortable.
Nasal aspiration is not considered an aerosol-generating procedure (AGP). Personal protective equipment when performing this procedure with suspected/confirmed COVID-19 patients should include contact (gown and gloves), and droplet (surgical mask) with eye protection.
Nasopharyngeal suction with a catheter
Use a catheter attached to a portable or wall suction source. After lubricating the catheter, gently advance it through the nostril and direct it toward the floor of the nasal cavity. Advance the catheter toward the lower pharynx, until the patient coughs or resistance is felt. At that point, apply suction and slowly remove the catheter.
Nasopharyngeal suction is considered an aerosol-generating procedure (AGP). Personal protective equipment when performing this procedure with suspected/confirmed COVID-19 patients should include contact (gown and gloves) and airborne (N-95 with goggles/face shield or PAPR) precautions.
The length of time a room should be shut down after an aerosol-generating procedure is dependent upon how many air exchanges occur per hour. If a room is not a negative pressure room, ideally the room should be shut down for 60 minutes before cleaning to allow tiny particles suspended in the air to settle.
See complete guide on how to hook up suction in your practice.
There are also several videos available online that manufactures of nasal suction devices have created.
Information for families
When should I bring my child back for bronchiolitis?
Your child should be seen for:
|
Difficulty breathing
|
|
|
Fever higher than 101 for more than five days |
|
 |
Signs of dehydration (no tears, dry mouth or fewer wet diapers) |
|
If you have any other concerns |
|
 |
Contact your child’s regular doctor or call the Children’s Mercy Nurse Advice Line: (816) 234-3188 Our Urgent Care locations are available for telehealth and in-person visits seven days a week:
|
 |
|
Cough and congestion may last for up to 14 days. Remember to follow up with your child’s health care provider if you believe additional care is needed.
Additional resources for your patients
The Respiratory Care team at Children’s Mercy has developed a guide for parents on how to use a manual nasal aspirator when providing suction for their infant at home. We encourage you to share this resource with your families:
We also have created patient information regarding bronchiolitis that you can find at Bronchiolitis Family Engagement Education and Suctioning for Bronchiolitis: FAQ for Parents.
For questions reach out to physicianservices@cmh.edu.
- Pulmonary and Sleep Medicine
- Advanced Asthma Interdisciplinary Respiratory (AAIR) Clinic
- Cystic Fibrosis Care Center
- Pediatric Pulmonology Fellowship
- Pulmonary Hypertension Clinic
- Respiratory Outpatient Clinic (ROC)
- Respiratory Outpatient Clinic: Update for Providers
- Sleep Center
- Sleep Medicine Fellowship
- PHIL Award Nomination Form
- Meet the Team