Anorectal Malformation (ARM)
What is an anorectal malformation?
When a baby is born with an absent, malformed, or displaced anus (the opening at the end of the digestive tract), this is called an anorectal malformation (ARM).
Issues with the anal opening include:
- Absent or missing anal opening (imperforate anus)
- Intestine empties into other pelvic structures – bladder, vagina
- Rectum, urologic, and/or reproductive systems share a common channel
- Small anal opening (cannot get poop out)
- Incorrectly placed anal opening (not surrounded by sphincter muscles)
When and why does it occur?
Anorectal malformation is a congenital defect that happens early in pregnancy, while a baby is still developing. It is believed to occur in 1 of 5,000 births. It is slightly more common in females than in males.
There is no one specific cause of ARM. Some patients may have a family history of ARM indicating a genetic component. Others have no family history. No environmental factors have been identified as contributing to ARM. In some instances, ARM is present with other birth defects as part of a syndrome such as VACTERL (vertebral, anorectal, cardiac, tracheoesophageal, renal and limb anomalies).
What are some types of anorectal malformations (ARMs)?
Male anorectal malformations
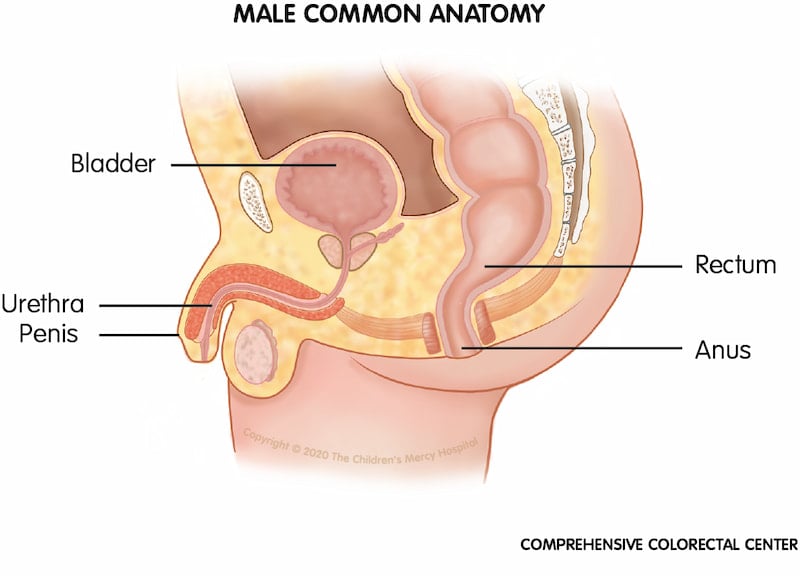
Common male anatomy. To compare variations in anatomy and structures for a male with an anorectal malformation, we have provided a picture of common anatomy for comparison.
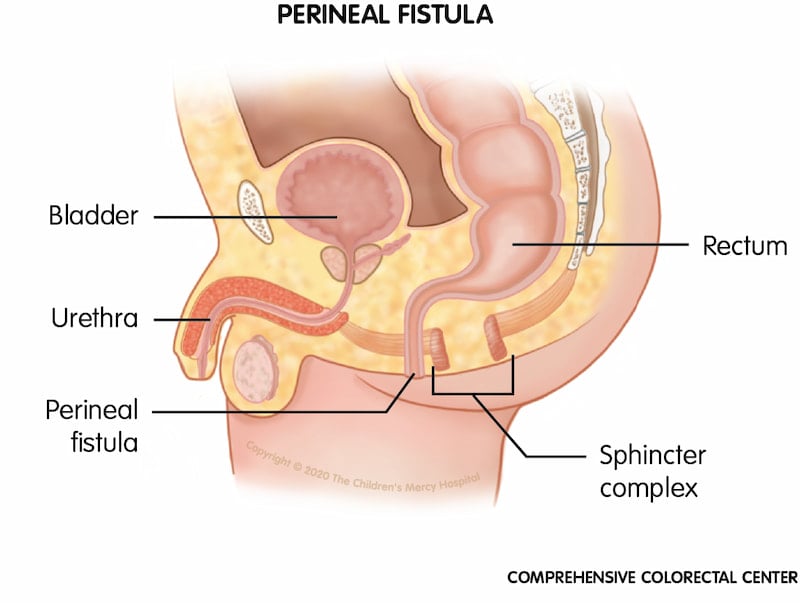
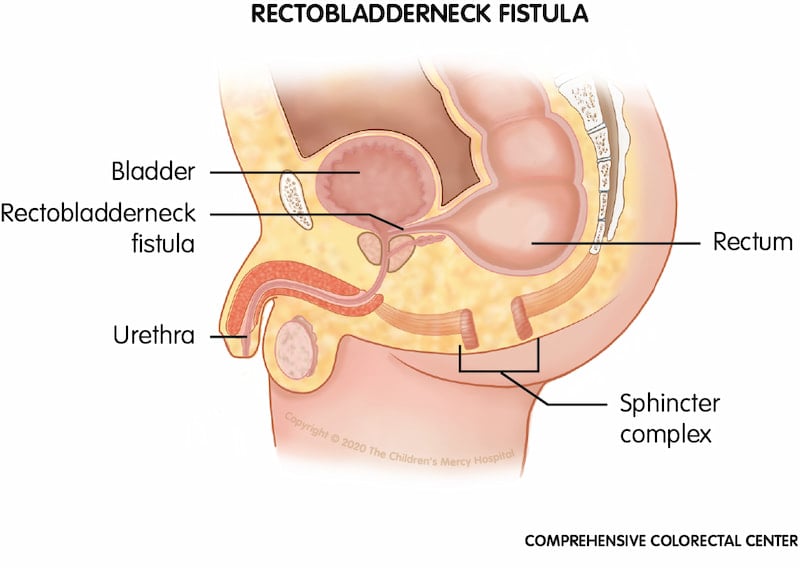
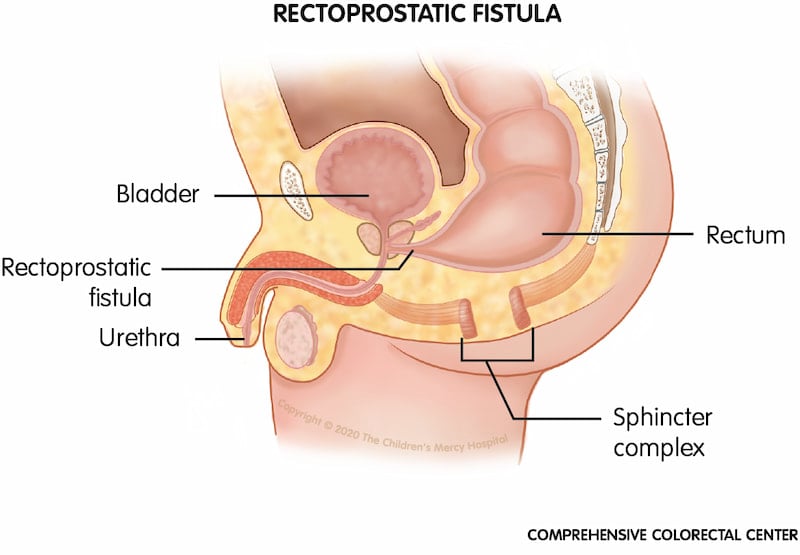
Some ARMs seen in males include:
Perineal fistula. When a baby is born with a perineal fistula, his rectum ends at an opening in the perineum (the space between the urinary and common anal opening area) instead of within the sphincter muscle complex of the anal opening.
Rectobladderneck fistula. When a baby is born with a rectobladderneck fistula, his rectum connects to the urethra, just below the bladder, instead of to the anus.
Rectoprostatic fistula. When a baby is born with a rectoprostatic fistula, his rectum connects to the urethra, near the prostate, instead of to the anus.
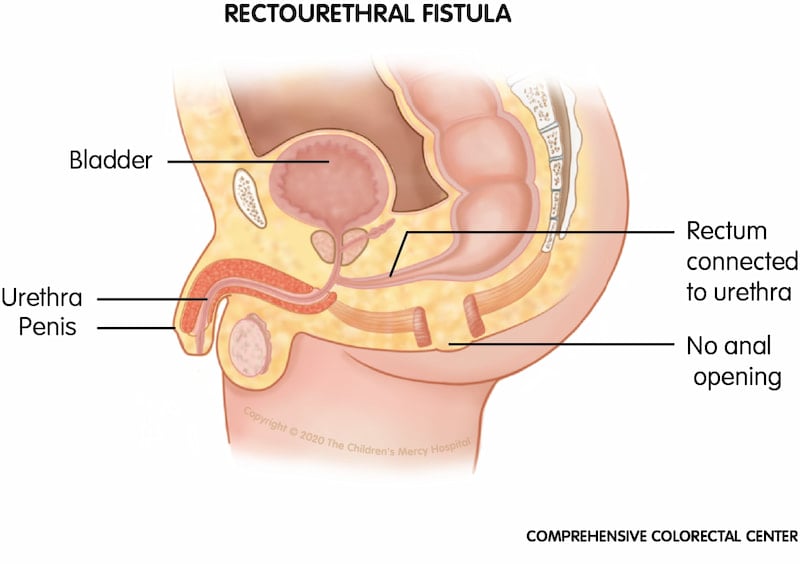
Rectourethral fistula. One of the most common male anorectal malformations (ARMs); when a male baby is born with a rectourethral fistula, his rectum is connected to the urethra instead of an anal opening.
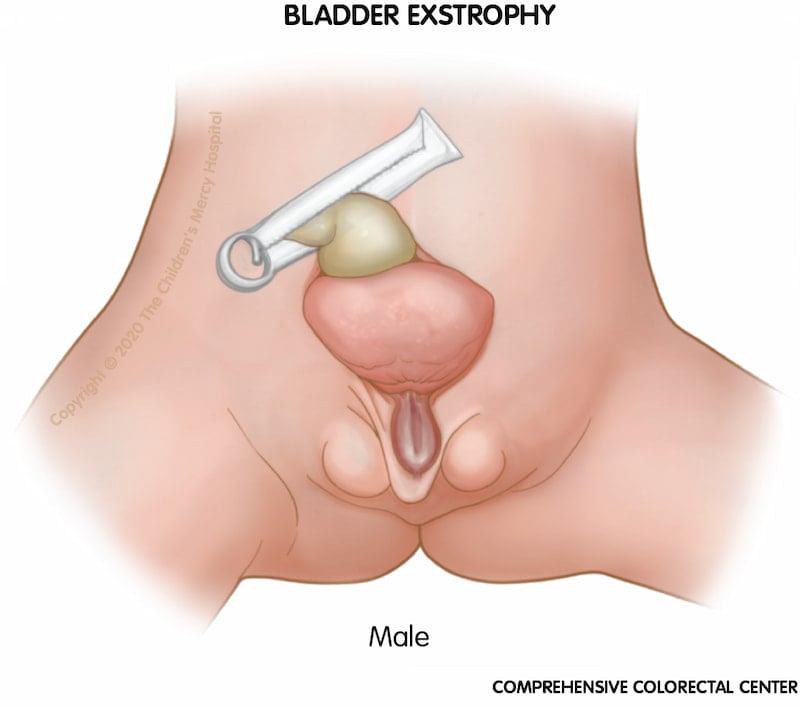
Bladder exstrophy. When a boy is born with bladder exstrophy, the bladder and urethra are open and seen as a divided structure (halves) on the outside of the body, the penis may be flat and short, and the top of the penis may open to the bladder.
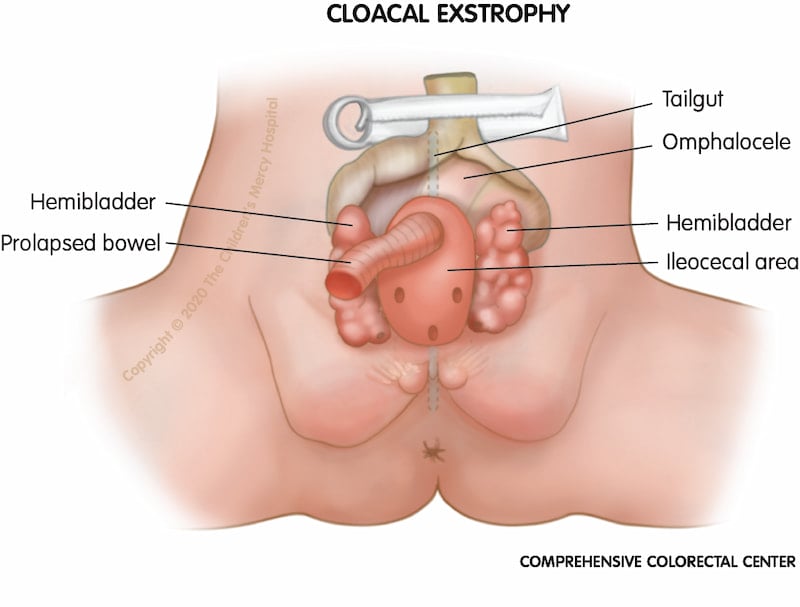
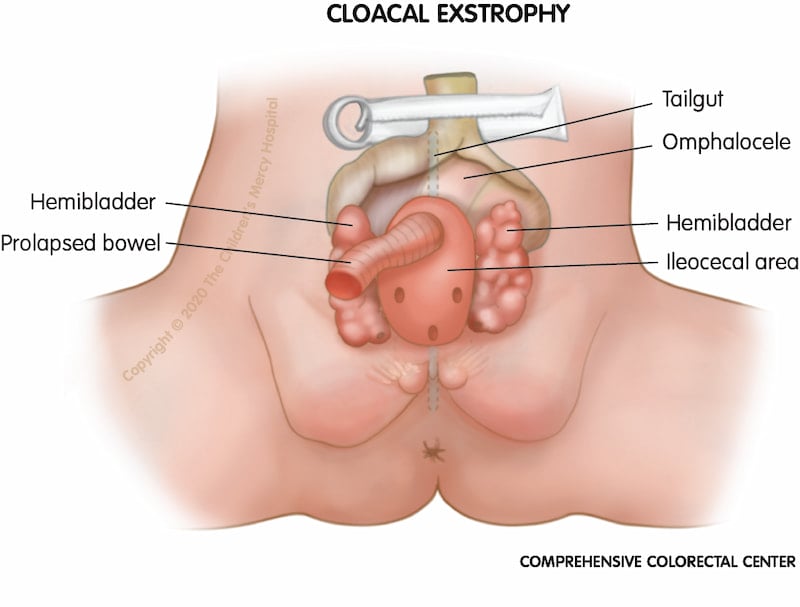
Cloacal exstrophy. When a baby is born with cloacal exstrophy, part of the intestines may be outside of the body (called omphalocele) and a portion of the small bowel called the terminal ileum may also stick out further, called prolapse. The small bowel (prolapse) comes out into the opened beginning part of the colon called the cecum. This means that poop does not come out of the anal opening (hindgut). The bladder may be outside of the body and in two pieces (called hemibladder). Urine (pee) drains directly onto the bladder plates through the ureters.
Female anorectal malformations
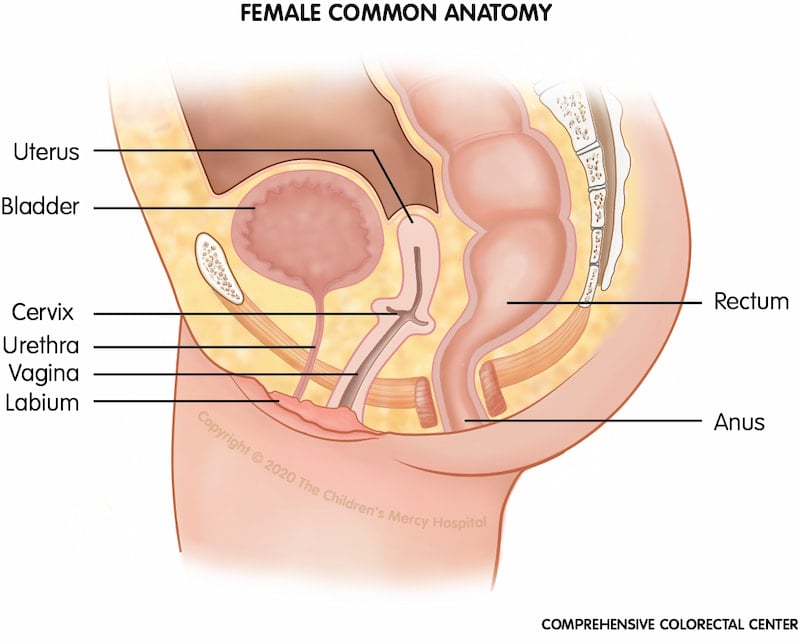
Common female anatomy. To compare variations in anatomy and structures for a female with an anorectal malformation, we have provided a picture of common anatomy for comparison.
Some ARMs seen in females include:
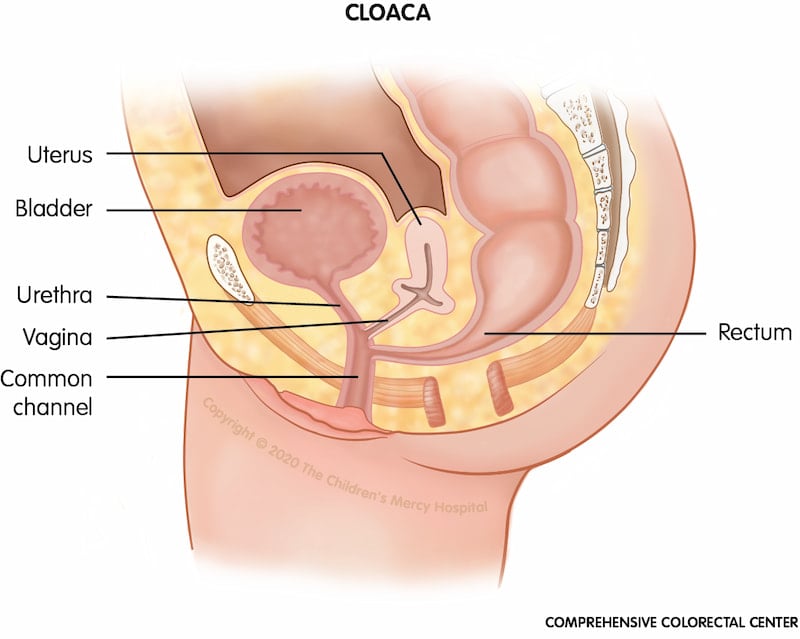
Cloacal anomaly or cloaca. Cloaca is a type of anorectal malformation in which the rectum, vagina and urinary tract are joined (waste, gynecologic and urinary structures are joined). This "common channel" ends in a single opening on the baby's bottom. The external private parts may look normal until closer inspection takes place.
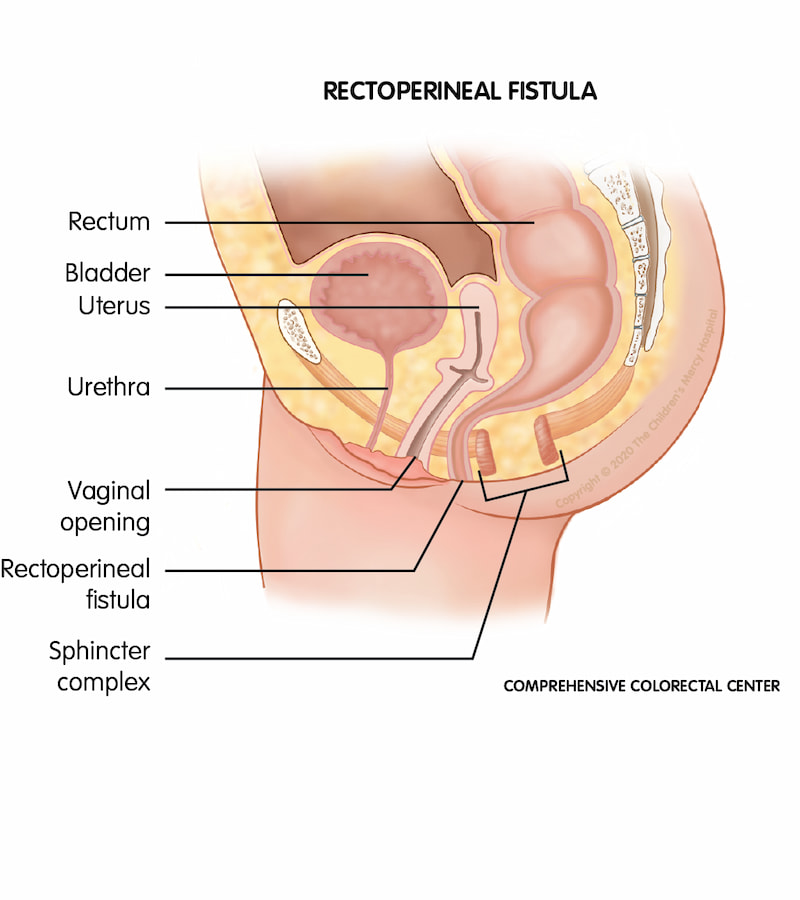
Rectoperineal fistula. When a baby is born with a rectoperineal fistula, the rectum ends at an opening in the perineum instead of the anus.
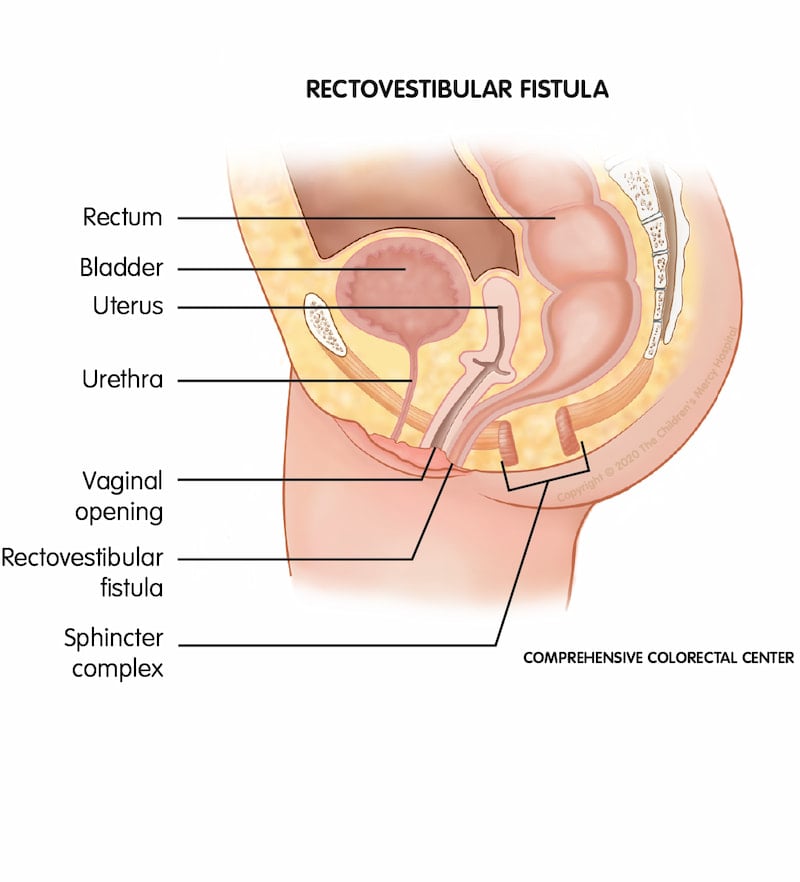
Rectovestibular fistula. One of the most common female anorectal malformations (ARMs); when a female baby is born with a rectovestibular fistula, her rectum exits near the vagina instead of through the anal sphincter muscle complex anal opening.
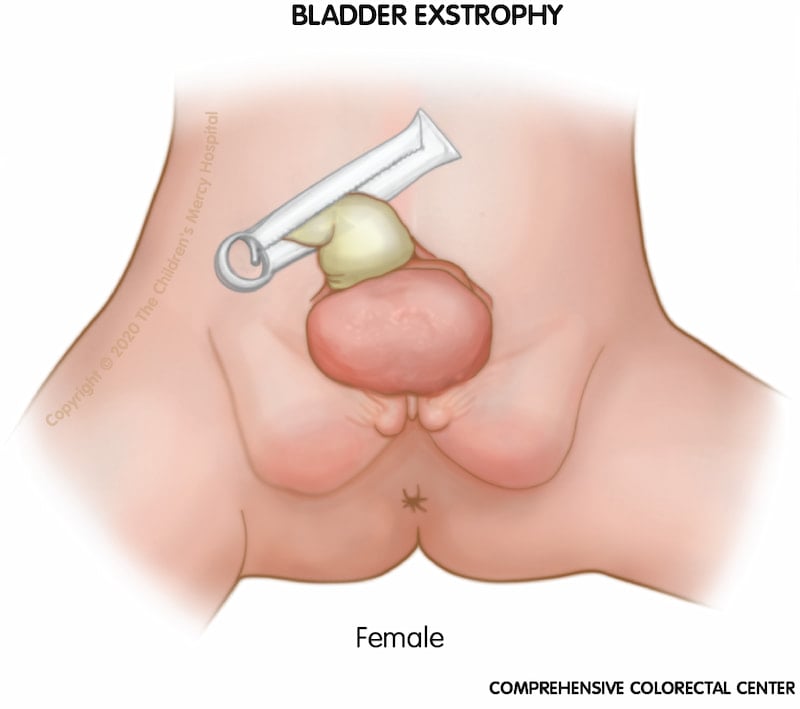
Bladder exstrophy. When a girl is born with bladder exstrophy, the bladder and urethra are open and seen as a divided structure (halves) on the outside of the body, and the clitoris may be separated into a right and left half.
Cloacal exstrophy. When a baby is born with cloacal exstrophy, part of the intestines may be outside of the body (called omphalocele) and a portion of the small bowel called the terminal ileum may also stick out further, called prolapse. The small bowel (prolapse) comes out into the opened beginning part of the colon called the cecum. This means that poop does not come out of the anal opening (hindgut). The bladder may be outside of the body and in two pieces (called hemibladder). Urine (pee) drains directly onto the bladder plates through the ureters.
How are anorectal malformations diagnosed?
Occasionally, anorectal malformations are diagnosed prenatally via sonogram; however, often this condition is not discovered until a baby is born, usually upon the initial physical exam or when there is no stool passed within the first 48 hours after birth.
Your doctor may order a number of tests to better understand your baby’s specific type of malformation and develop a plan.
These tests may include:
- Abdominal X-rays to see how the lower backbone has developed
- Abdominal ultrasound to evaluate the kidneys, urinary structures and how urine (pee) is draining
- Spinal ultrasound or spinal MRI to evaluate for tethered spinal cord
- Echocardiogram (ECHO) to look for heart defects
- High pressure distal colostogram – a contrast study done prior to surgical reconstruction at 3 months of age if your child had a colostomy created
What are the symptoms of anorectal malformation?
Aside from the missing or displaced anus, the most obvious concern is that the baby is not able to pass stools normally. Newborns should pass their first stool within 48 hours. If this does not occur, further testing may be performed to determine the cause of the issue. Not being able to pass stool normally from the colon can cause constipation, pain, infection and damage to the colon.
What are anorectal malformation care options?
Special types of surgery are required to repair anorectal malformation. In some instances, multiple surgeries spaced over several weeks or months may be required in order to completely repair the malformation.
Often the first surgery in this series is done to direct solid waste from the colon to an external bag (colostomy). This procedure greatly reduces the risk of infection for future reconstructive procedures.
These surgeries require a skilled multidisciplinary team including specialists from the colorectal center, gynecology, urology, gastroenterology, and orthopedics, coordinated through the Comprehensive Colorectal Center.
What does surgery for anorectal malformation look like?
- First doctors will look to make sure your baby can safely get poop out of their body. If they can get poop out, your child may be able to either go home and come back for a later surgery or get a surgery when they are very young.
- If poop cannot safely come out, then a temporary colostomy may be recommended.
- A few months after the colostomy has been placed, the surgery for the ARM takes place called a posterior sagittal anorectoplasty (PSARP) or anoplasty.
- Your surgeon will discuss the best minimally invasive surgical approach with you. The last surgery is closing the colostomy and letting poop come out of the newly created anal opening.
Anorectal Malformation - Posterior Sagittal Anorectoplasty (PSARP)
What is posterior sagittal anorectoplasty (PSARP)?
At approximately 3 months old, doctors may perform a type of pull-through procedure called a posterior sagittal anorectoplasty (PSARP).
What is the goal of PSARP?
The goal of the PSARP procedure is ultimately to create an anus so the child can safely poop.
How is the PSARP procedure performed?
During a PSARP procedure, the surgeon creates an anus within the child’s sphincter muscles, resulting in an opening from which the child can poop. Because the child may have had a colostomy at birth, a few weeks later, the colostomy is closed, allowing the child to poop out of the new anal opening.
Your child’s doctor may recommend anal dilation following surgery to prevent scar tissue from forming that could narrow the opening. Our team then follows the child with periodic anatomy checks to make sure the surgery heals properly and that the child’s development is on track.
What are the benefits of the PSARP procedure?
The PSARP procedure helps create a more normal anatomy so the child can poop safely.
What to expect at the Comprehensive Colorectal Center
The Comprehensive Colorectal Center always strives for the best possible outcome for each individual patient.
Surgical procedures are designed to restore potential function. However, since absent or under-developed neurological and muscular structures are often a part of an anorectal malformation, many children will need some additional assistance in controlling their bowel movements or may struggle with constipation.
These children can benefit from a structured bowel management program once they are ready to toilet train. The Comprehensive Colorectal Center offers these programs via our Bowel Management Boot Camp or individual clinic visits.
Children with more complex syndromes affecting other body systems will need long-term management from a diverse care team, possibly including specialists in nephrology, orthopedics, and gastroenterology.
Call for an appointment
We're here to help you. Contact us for more information about the Comprehensive Colorectal Center at Children's Mercy.
- Colorectal Center
- Speak With Our Team
- Comprehensive Colorectal Care
- Conditions and Treatments
- Bowel Management Boot Camp
- Colorectal Surgery
- Resources for Caring for Colorectal Conditions at Home
- Insurance Information
- Advancing Care Through Research
- What to Expect
- Meet the Team
- General and Thoracic Surgery
