Cloacal Exstrophy
What is cloacal exstrophy?
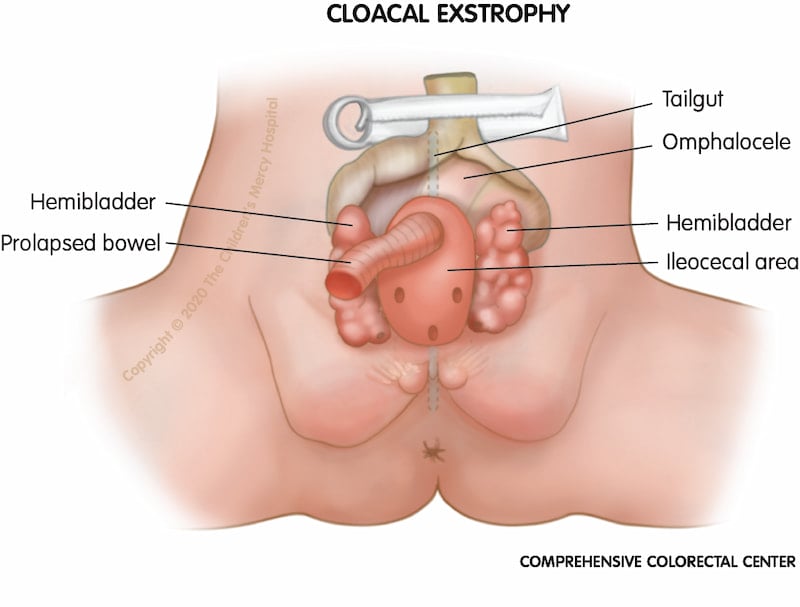
When a baby is born with certain inner abdominal organs and structures exposed on the outside of the abdomen, along with some malformation of these organs, this is called cloacal exstrophy.
Some common characteristics of cloacal exstrophy are:
- A large portion of the intestines may lie outside the body, protruding through the umbilical cord area (omphalocele)
- On either side of the exposed intestines are the two halves of the bladder
- In males the penis may be flat and short, and each penile half may be separated
- In females the clitoris may be separated into a right and left half
Call for an appointment
We're here to help you. Contact us for more information about the Comprehensive Colorectal Center at Children's Mercy.
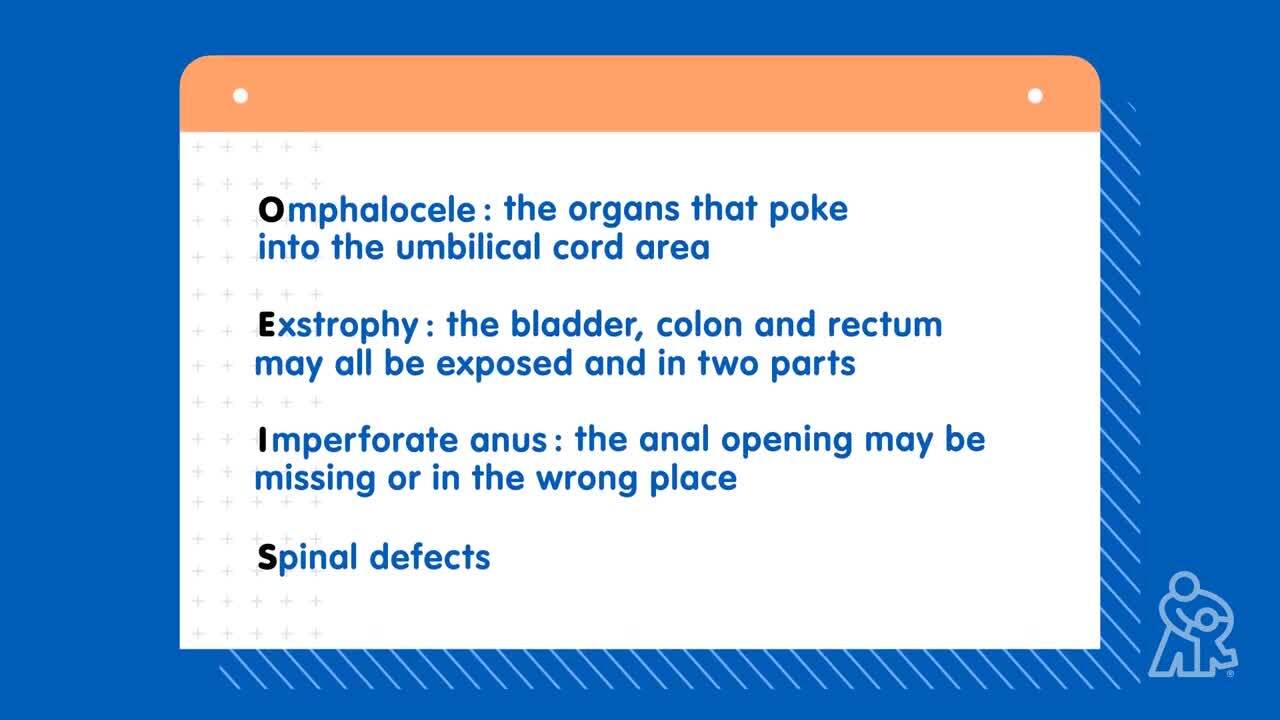
Cloacal exstrophy is also known as OEIS
OEIS stand for a combination of conditions that are often present together:
- Omphalocele – Some of the abdominal organs protrude through the umbilical cord area. The omphalocele may be small – involving only some intestines – or may be large and contain other abdominal organs such as the liver.
- Exstrophy of the bladder and rectum – The bladder is open and separated into two parts. The colon and rectum may also be divided.
- Imperforate anus/anorectal malformation – The anal open may be in the incorrect location or be missing entirely.
- Spinal defects – These may be minor or major and may include spina bifida, which is the incomplete closure of a section of the spine and membranes surrounding the spinal cord.
When and why does it occur?
Cloacal exstrophy is a very rare congenital defect that happens early in pregnancy, while a baby is still developing in the uterus. It is believed to occur in approximately 1 of 250,000 births.
There is no one specific cause of cloacal exstrophy. Some patients may have a family history of cloacal exstrophy indicating a genetic component. Others have no family history. No environmental factors have been identified as contributing to cloacal exstrophy.
How is this condition diagnosed?
Often, cloacal exstrophy is diagnosed prenatally via sonogram; however, sometimes this condition is not discovered until a baby is born.
Your doctor will order several tests to better understand your baby’s specific type of malformation and develop a plan.
These tests may include:
- Abdominal X-rays
- Abdominal ultrasound to evaluate the kidneys, urinary structures and how urine (pee) is draining
- Spinal ultrasound or spinal MRI to evaluate for tethered spinal cord
- Echocardiogram (ECHO) to look for heart defects
What is the treatment for cloacal exstrophy?
Cloacal exstrophy requires a series of surgeries, also known as ‘staged reconstruction’. These will be planned and prioritized based on the types and severity of malformations listed below.
- Priority is to make sure:
- Poop can exit the body safely
- Urine can exit the body safely
- Organs such as intestines which may be exposed and visible are protected
What are some of the surgeries for cloacal exstrophy?
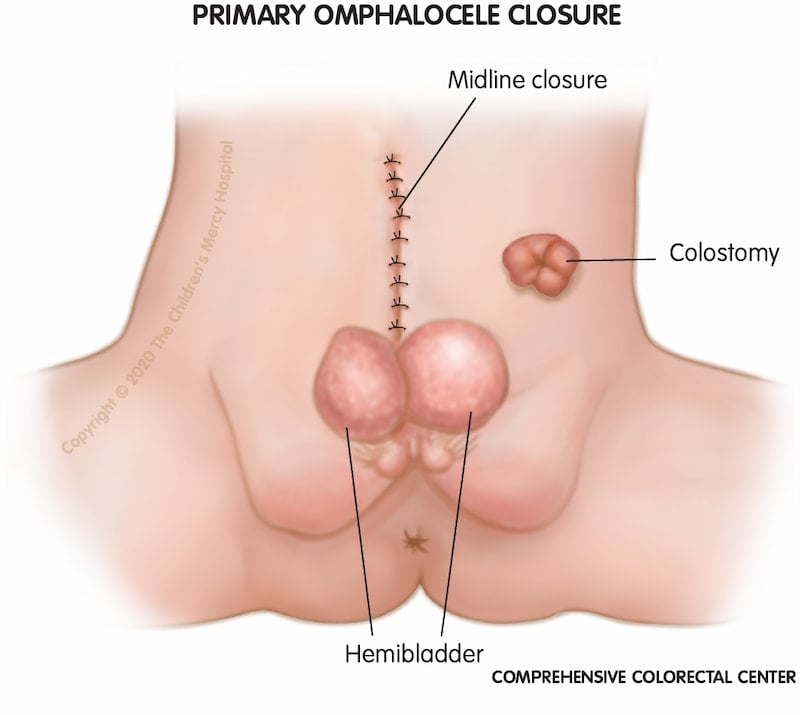
Abdominal repair: The first stage of surgery may also be called omphalocele closure. The abdominal wall may not be able to close completely and may be closed in stages. Often when the abdominal wall is closed, the two sides of the bladder are brought closer together. The end of the colon is located and a colostomy is made which lets poop exit your baby’s body. During this surgery, the urology team evaluates if urine can exit the body safely as well as moves the open bladder halves closer together (called bladder exstrophy) During this stage, the urology team also makes sure that there is a way to safely urinate and monitor the urinary system.
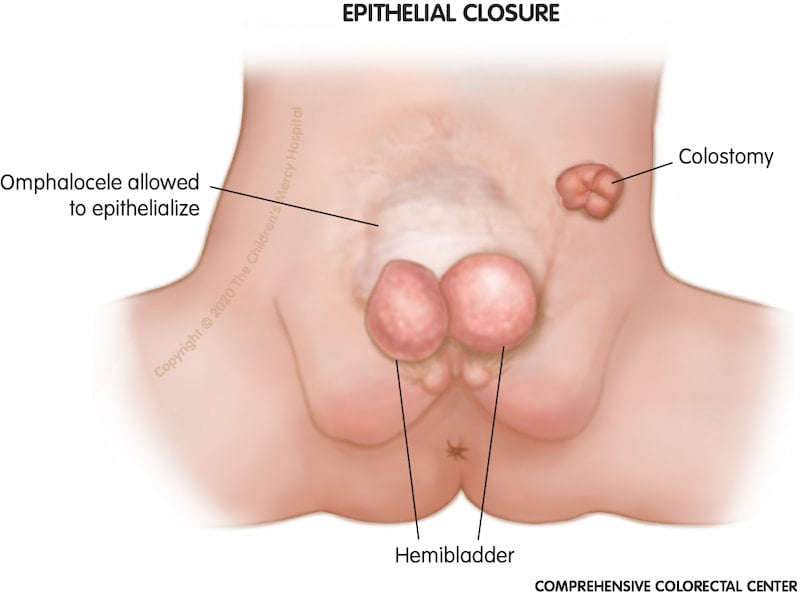
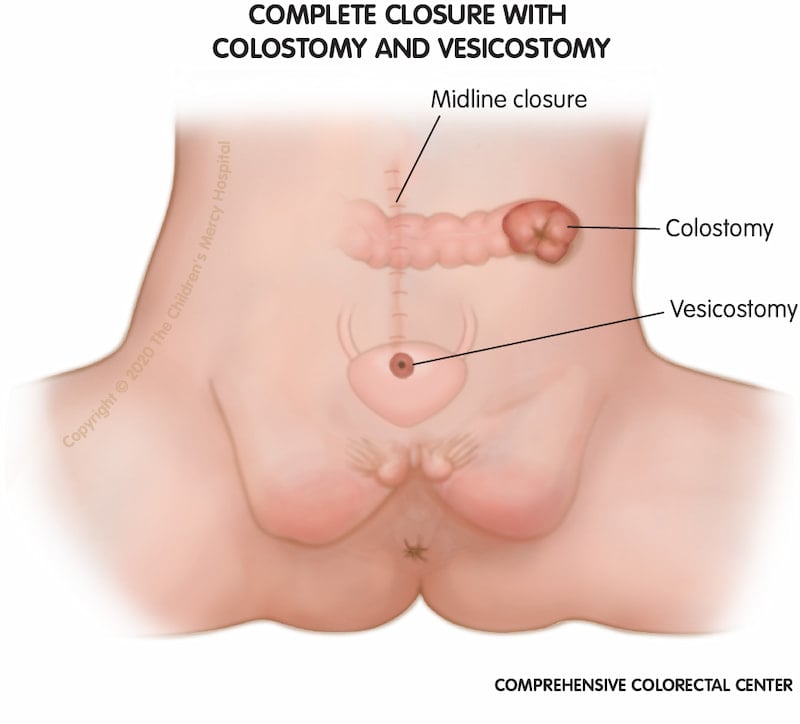
Osteotomies: Once your child has healed, the second stage of surgery involves working on the bladder (and sometimes the abdominal wall if it is not completely closed). The bladder is brought together by a urologist and tucked into the abdomen. The orthopedic surgery team helps to bring the pelvic bones closer together (by performing a procedure called an osteotomy) as they can be further apart. Children who need osteotomies may be placed in traction or a spica cast for a few weeks after surgical repair.
Pull-through procedure: Many families wonder if their child will have the ability to poop out of their bottom instead of having a colostomy bag. This reconstruction is usually done later. The surgery involves having poop come out of the bottom instead of into a colostomy bag. This surgery depends on the amount of colon and the thickness of your child’s stool. Our team can help assess if your child can have this surgery.
Spinal surgery: Depending on the spinal development of your child, spinal surgery may be required. A neurosurgeon performs this surgery.
Additional surgeries: Children are followed life-long to ensure the health of the bladder, kidneys, bowel, spine, heart and reproductive organs. There will be additional testing to see how these organs are doing during your child’s growth and development. Additional treatment, surgeries and procedures are commonly recommended to help improve your child’s quality of life and independence.
What are cloacal exstrophy care options?
Because cloaca exstrophy involves multiple body systems, children do best when their care is provided by a coordinated team of experts in colorectal surgery, gynecology, urology, orthopedic surgery, neurosurgery and radiology, such as is available at the Children's Mercy Comprehensive Colorectal Center.
- Colorectal Center
- Speak With Our Team
- Comprehensive Colorectal Care
- Conditions and Treatments
- Bowel Management Boot Camp
- Colorectal Surgery
- Resources for Caring for Colorectal Conditions at Home
- Insurance Information
- Advancing Care Through Research
- What to Expect
- Meet the Team
- General and Thoracic Surgery