Cloacal Anomaly or Cloaca
What is cloaca?
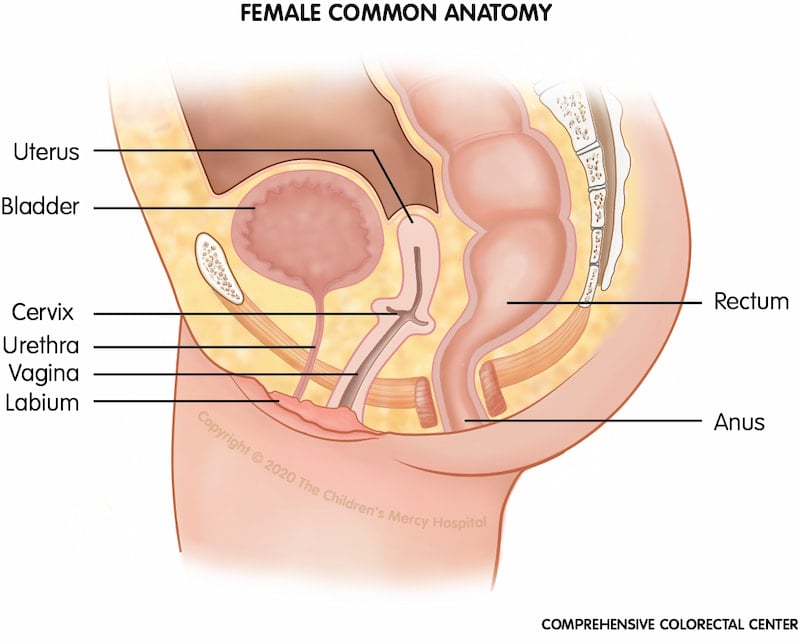
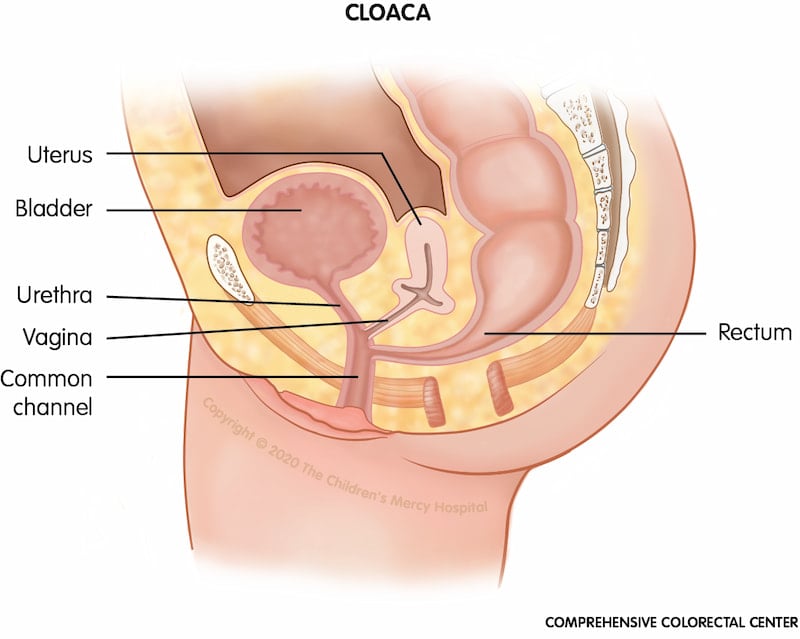
Cloaca is a type of anorectal malformation (ARM) in which the rectum, vagina and urinary tract are fused together. The location where these structures (gynecologic, urologic and colorectal) all join together is called the "common channel." This common channel ends in a single opening on the baby’s bottom (perineum).
When and why does cloaca occur?
Cloaca is a rare congenital defect that occurs in 1 in every 20,000 to 25,000 newborn females. It occurs very early in the baby’s development in the uterus.
There is no one specific cause of cloaca. Some patients may have a family history of ARM indicating a genetic component. Others have no family history. No environmental factors have been identified as contributing to cloaca. In some instances, cloaca is present with other birth defects affecting the bones of the lower back, the kidneys, or the reproductive organs.
How is cloaca diagnosed?
Occasionally, cloaca is diagnosed prenatally (before birth) via sonogram or ultrasound; however, often this condition is not discovered until a baby is born, usually upon the initial physical exam.
There are variations in the location of the common channel and your doctor will order tests to better understand your baby’s specific type of malformation and develop a plan.
These tests may include:
- Abdominal X-ray(s) and bowel contrast study
- Abdominal ultrasound to evaluate the kidneys, gynecologic, and urinary structures and how urine (pee) is draining from the kidneys, bladder and vagina (an issue called hydrocolpos)
- Spinal ultrasound or spinal MRI to evaluate for tethered spinal cord
What are the symptoms of cloaca?
Babies with a cloacal anomaly have only one opening in the perineum (bottom), and if left untreated, this condition can lead to problems with passing urine and stool, intestinal blockage or perforation, abdominal cysts and urinary tract infections. Urine can back up into the kidneys leading to kidney damage. Later in life, sexual function and the ability to give birth may be compromised.
How is cloaca treated? Will surgery be needed?
Cloaca anomalies are treated with a colostomy soon after birth to divert stool away from the urinary and gynecological systems. Your child’s urinary and gynecologic system will also be carefully evaluated to make sure that urine is draining well from the kidneys/bladder and vaginal structures. Occasionally, this requires additional procedures and/or surgery.
Following the newborn period, your child is followed by careful assessment and surgery, through the combined services of pediatric experts, including colorectal surgery, gynecology, urology and radiology.
Long term follow-up with a team that understands cloaca is very important. These complex surgeries are best done with the help of a multidisciplinary team such as the one available at the Comprehensive Colorectal Center.
Cloaca Reconstruction - Posterior Sagittal Anorectal Vaginal Urethral Plasty (PSARVUP)
What is posterior sagittal anorectal vaginal urethral plasty (PSARVUP)?
At approximately 5 months old, pediatric experts, including colorectal surgery, gynecology, urology and radiology, carefully examine the child’s anatomy to determine if the child needs a cloaca reconstruction procedure called a posterior sagittal anorectal vaginal urethral plasty (PSARVUP). Another type of cloacal surgery that accomplishes the same outcome is called a total urogenital mobilization (TUM). Your child’s surgeon will discuss the type of operative repair that is best for your child’s anatomy and outcomes.
This surgical procedure separates the three joined openings into three separate ones.
What is the goal of PSARVUP or TUM?
The goal of the PSARVUP procedure is to create three separate structures, a urethra, a vagina and an anus, so the child can safely pee and poop.
How is the PSARVUP or TUM procedure performed?
During a PSARVUP or TUM procedure, the three joined openings created by the cloacal defect are separated into three distinct openings. The result is a more normal anatomy so the child has a urethra, a vagina and an anus. Because the child typically has had a colostomy at birth, a couple of months later, the colostomy is closed, allowing the child to poop out of their bottom. Depending on your child’s anatomy, laparoscopy (minimally invasive surgery) can be utilized to decrease the number of large incisions.
Our team then follows the child with periodic anatomy checks to be sure the reconstruction heals properly and that the child’s development is on track. Some children with cloaca struggle with potty training, and some need additional reconstructive surgeries later.
What are the benefits of the PSARVUP or TUM procedure?
The PSARVUP procedure helps create a more normal anatomy so the child can pee and poop safely. Long term, this procedure also makes normal female sexual and reproductive functions possible.
Follow-up with a team that understands cloaca is very important. These complex surgeries are best done with the help of a multidisciplinary team such as the one available at the Comprehensive Colorectal Center.
What to expect at the Comprehensive Colorectal Center?
The Comprehensive Colorectal Center always strives for the best possible outcome for each individual patient. Surgical procedures are designed to restore potential function; however, since absent or under-developed neurological and muscular structures are often a part of a cloaca, many children will need some additional assistance in controlling their bowel movements or may struggle with constipation. These children can benefit from a structured bowel management program once they are ready to toilet train. The Comprehensive Colorectal Center offers these programs via our Bowel Management Boot Camp or individual clinic visits.
Children with more complex syndromes affecting other body systems will need long-term management from a diverse care team, including specialists in nephrology, orthopedics, and gastroenterology.
Call for an appointment
We're here to help you. Contact us for more information about the Comprehensive Colorectal Center at Children's Mercy.
- Colorectal Center
- Speak With Our Team
- Comprehensive Colorectal Care
- Conditions and Treatments
- Bowel Management Boot Camp
- Colorectal Surgery
- Resources for Caring for Colorectal Conditions at Home
- Insurance Information
- Advancing Care Through Research
- What to Expect
- Meet the Team
- General and Thoracic Surgery