Pectus Excavatum
What is pectus excavatum?
If your child develops a sunken chest — referred to as pectus excavatum — it is likely that another family member has had the condition too. While we don't know the exact causes of pectus excavatum, the condition tends to run in families. About 25 percent of children with this condition discover a family history of others with “funnel chest” (also known as caved-in chest).
Pectus excavatum is the most common difference in children’s chest walls and can become visible anytime from infancy through puberty. Pectus excavatum occurs in about 1 in 1,000 children and boys are 4 times more likely to have this condition than girls.
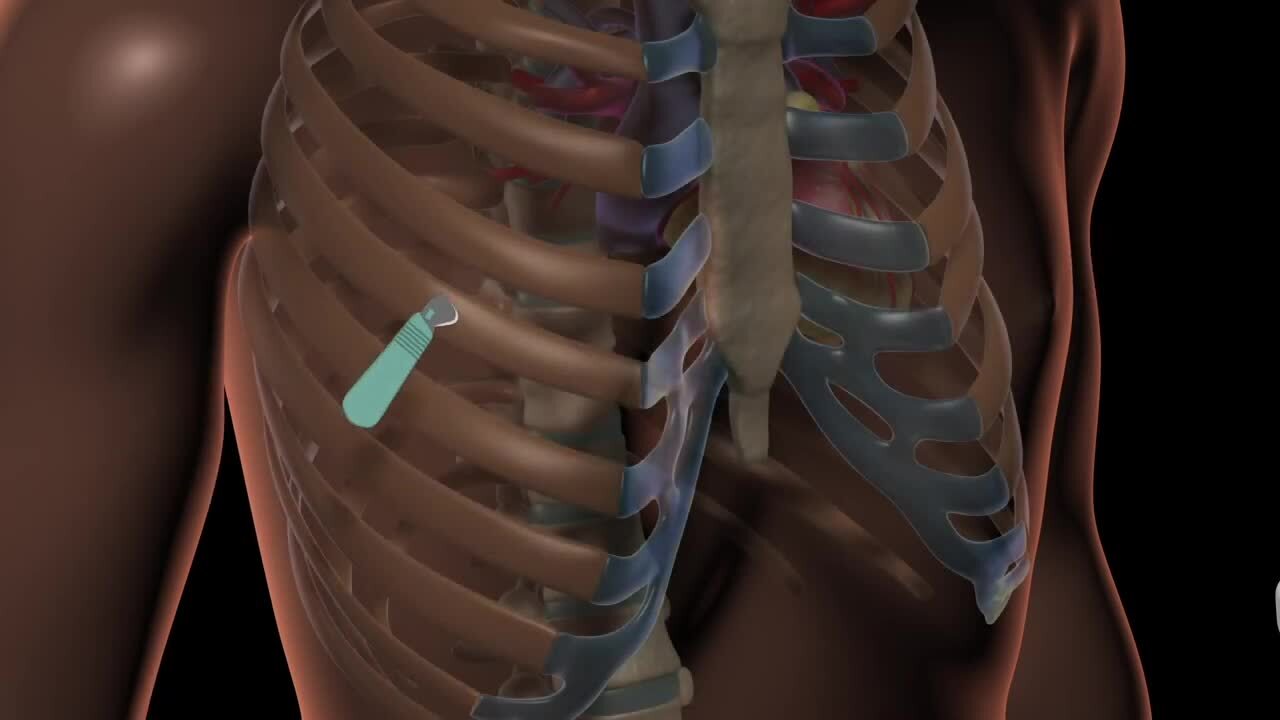
Pectus excavatum occurs when several ribs and the sternum (breastbone) don’t grow normally, causing the sternum to be pressed inward. This results in a sunken spot, or depression, that is visible when looking at your child’s chest. The depression can range in size and depth. Sometimes it is deeper on one side, causing the breastbone to be curved. In severe cases, the depression is so deep that it pushes the sternum to nearly touch the spine. Pectus excavatum can cause physical difficulties as well as social and emotional challenges in some children.
Some children who have pectus excavatum also have scoliosis, although one doesn’t necessarily cause the other.
Symptoms of pectus excavatum
Symptoms often include:
- Shortness of breath
- Chest pain
- Exercise intolerance
- Body image issues
Stay active while living with pectus excavatum
Encourage your child to live an active lifestyle without any restrictions, unless your care team recommends otherwise. People who have pectus excavatum can continue to participate in all activities they find enjoyable.
Some symptoms may get worse with physical activity but the activity itself does not pose a health risk. Pay attention to activities that seem to cause problems and ask your child's pectus team if there is any relation.
Treatment options for pectus excavatum
Pectus excavatum typically becomes more noticeable during puberty when your child begins to grow rapidly.
Adolescents with a severe case of pectus excavatum and associated symptoms may be a candidate for surgical repair during the teenage years with the minimally invasive repair of pectus excavatum (MIRPE).
Vacuum Bell Therapy (VBT) offers a nonsurgical treatment option for pectus excavatum. VBT uses a suction device to gradually lift the sternum/chest wall. Correction using VBT typically does not improve the appearance of the chest as much as surgical correction. However, for some children, VBT represents a potential alternative to surgery.
Testing for pectus excavatum
Your pectus care team may recommend a chest CT (CAT scan) of your child's chest to determine how severe their condition is. The CT scan can measure the indented chest depression and help your care team to determine the best treatment option for your child. The CT scan is not painful and simply requires your child to lie still for about 5-10 minutes while a series of pictures are taken.
Additional testing (such as an exercise stress test, pulmonary function tests or an echocardiogram) may be required by your insurance company if you are considering surgery. Sometimes, surgery is not covered by insurance. We recommend checking with your insurance company for specifics.
Pectus excavatum surgery: Nuss procedure and MIRPE
Minimally invasive repair of pectus excavatum (MIRPE)
Doctors began using open surgery to correct pectus excavatum in the early 1900s. Eighty years later, Donald Nuss, MD, a Norfolk, Va. doctor, came up with an approach that was less invasive. Since then, the surgeons at Children’s Mercy have modified the Nuss procedure to include a central incision that allows safe passage of the bar across the chest.
During the MIRPE procedure, the surgeon inserts a steel bar that has been bent to fit under the sunken sternum and around the front of the chest. The bar helps reshape the chest as the child grows.
After about three years, the bar is removed in a same-day procedure. This pectus excavatum repair is highly effective. Less than 1 percent of children will develop the condition again.
Using cryoablation to reduce pain after surgery
Cryoablation is a newer method of pain management for people undergoing bar placement to repair pectus excavatum. It can dramatically reduce pain after surgery. Extensive research on cryoablation revealed that cryoablation was safe and effective to improve pain control and shortened the hospital stay.
In the operating room, the surgeon will freeze 4 nerves that run between the ribs on each side prior to placing the bar. This will temporarily decrease pain transmission through these nerves. It may take 12-24 hours for optimal pain control.
It's important to know that cryoablation does not eliminate the pain completely. The effects of cryoablation will last between 2-3 months. Your child may experience some skin numbness in the chest wall. The numbness should get better within 3-6 months when the nerve grows back and regains function.
Your child will go home with short-term oral pain medications to continue during their recovery. Most children can go home the day of surgery.
What to expect after pectus surgery
Your child will not need any stitches removed because doctors will have closed the incisions using dissolving stitches under the skin. Steri-strips bandages will be in place on the skin and fall off on their own in about 2 weeks. The incisions will be pink and gradually fade over the next year. We recommend keeping sunscreen on the scars for improved healing.
Pain control
- Some pain is expected.
- Most children experience postoperative discomfort in the form of intense pressure because of the force the bar puts on the sternum (breastbone). This will improve with time.
- Be very mindful with your pain medication regimen, pain control activities and other prescribed medications.
- It is important to take the scheduled Tylenol and ibuprofen for the first 3 days even if not in pain.
- Pain control from cryoablation should reduce your child's need for additional pain medications after the first few days after surgery.
Follow-up appointments
Most families will have a follow-up visit 2 weeks after surgery and then as needed until it is time for bar removal.
Activity level after surgery
Follow these guidelines to help your child recover and gradually return to normal activities after surgery:
-
No strenuous physical activity for 2 weeks following surgery.
-
May return to normal activity as tolerated after 2 weeks, including sports. We recommend slowly increasing activities and easing into heavy lifting and contact sports.
- Although there are not specific activity restrictions, your child may find that certain activities are more uncomfortable than others. It's a good idea to avoid those for as long as it takes to be able to do them comfortably.
Returning to school
Your child can return to school when their energy level improves and pain is well-controlled. Your child should not drive if they have taken Oxycodone.
Medical concerns while the bar is in place
-
No dental prophylaxis or antibiotics needed prior to dental procedures if you have a pectus bar in place.
- "What's that noise?"
- A popping or clicking sound or sensation is normal and can occur with movement of the bar and/or stabilizer within the chest wall. This may occur occasionally throughout the time the bar is in place.
- A popping or clicking sound or sensation is normal and can occur with movement of the bar and/or stabilizer within the chest wall. This may occur occasionally throughout the time the bar is in place.
-
No MRI examinations of the chest and abdomen are allowed. CT scans are acceptable.
-
If defibrillation is needed, paddle placement needs to be anterior/posterior (front and back).
-
CPR CAN BE PERFORMED but may require more exertional external force from the rescuer.
-
We recommend a medic alert bracelet. Inscription should state: “surgical steel bar in chest.” You can find these at American Medical ID.
What to do if you have concerns
If you have a question, you can send a message to the Pectus Center through the patient portal or call the Surgery Clinic at (816) 234-3097. Please contact us if your child is experiencing any of the following concerns:
-
The incision becomes red, swollen, very painful or begins draining or a rash develops.
-
You think the bar has become dislodged (the chest changes shape or your child has been hit forcefully in the chest).
-
Your child has new pain that is not responsive to over-the-counter pain medications.
Inside Pediatrics: Jacob's story
Revolutionary cryoablation procedures pioneered at Children’s Mercy allow Jacob to recover with almost no discomfort from a chest repair that used to cause months of pain.
Highest level of surgical care
Children’s Mercy is one of only 53 centers in the nation to be verified as a Level 1 Children’s Surgery Center — the highest possible rating — by the American College of Surgeons. This verification means Children's Mercy meets the highest standards for safety and outcomes determined by the American College of Surgeons. Our surgical care is designed to manage routine to highly complex illnesses. We also have experts in every pediatric specialty ready to go at all times to provide comprehensive care for kids.
Planning for surgery
From free valet parking at the front door to personalized follow-up care during your child’s recovery, we want every aspect of your experience at Children’s Mercy to be beyond your expectations.
Read about how to prepare your child for scheduled surgery, what to expect when you arrive, and resources available while you’re here.
Pediatric anesthesia at Children's Mercy
At Children’s Mercy, a pediatric anesthesiologist is an active member of your child’s care team before, during and after their surgery or procedure.
We administer anesthesia for more than 27,000 kids per year—that’s 74 per day—so our team is experienced at finding just-right doses of medication for kids of all sizes.