Eyelid Swelling: What's the Diagnosis?
Visual Diagnosis - February 2023
Column Author: Ronald Palmen, MD | Internal Medicine-Pediatrics Resident, PGY 3
Column Editor: Joe Julian, MD, MPHTM | Hospitalist, Internal Medicine-Pediatrics; Clinical Associate Professor, Internal Medicine & Pediatrics
A 6-year-old previously healthy female is admitted directly from a referring emergency department (ED) in the community for further evaluation and management of right eyelid swelling. Patient was in normal state of health until one week before presentation when she developed cough, nasal congestion, body aches, and fevers up to 102-103 F. Her parents sought care with their primary care provider two days prior, where she was diagnosed with influenza A and oseltamivir was prescribed. The patient developed rash on her face, chest, neck and upper back after starting the medication. Later that evening, she was noted to have right eyelid swelling, which her parents attributed to allergies. The following morning, the patient woke up with worsening swelling and right eye pain. She was seen in her local ED and referred for admission based on her examination and CT imaging.
Vital signs are notable for a temperature of 101.8 F. Labs are notable for a white blood cell count of 27,700 (74% neutrophils, 25% bands). Examination is notable for extensive edema and erythema of the right eyelid with difficulty visualizing the globe. Patient has pain with eye movements, and purulent drainage is noted along the eyelid. Sandpaper-like rash is present on her face, upper chest, arms and back. Purulent drainage is present in right nares.


QUESTION #1
What is the most likely diagnosis for this patient?
- Preseptal cellulitis
- Orbital cellulitis
- Allergic conjunctivitis
- Dacryocystitis
ANSWER #1
B. Orbital cellulitis
While preseptal and orbital cellulitis can have similar presentations, their clinical course differs due to the location of the infection. Preseptal cellulitis includes inflammation of soft tissues anterior to the orbital septum, whereas orbital cellulitis includes the deeper tissues including fat and muscles within the orbit, excluding the globe.
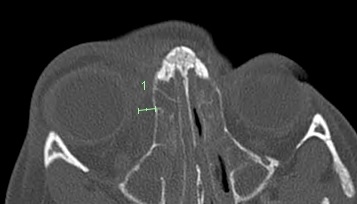
In this case, a few clinical features raise concern for orbital cellulitis. Pain with eye movement and upper eyelid edema without brow involvement (further edematous spread limited by orbital septum) point toward the more serious diagnosis of orbital cellulitis. This diagnosis is confirmed by imaging, which additionally shows a subperiosteal abscess along the right lamina papyracea (see green measurement).
It is important to differentiate these diagnoses via imaging studies if physical examination is indeterminate (often because the patient’s eyelids are too edematous and painful to be completely evaluated without ophthalmologic assistance). The most commonly used imaging modalities are contrasted computed tomography and magnetic resonance imaging.
QUESTION #2
For this patient, which is the most appropriate intravenous empiric antibiotic selection?
- Vancomycin
- Ceftriaxone
- Ampicillin-sulbactam
- Piperacillin-tazobactam
ANSWER #2
C. Ampicillin-sulbactam
Orbital cellulitis is most commonly due to streptococcal and staphylococcal species, with Haemophilus influenzae type b previously being a large contributor prior to the Hib vaccine. Initial antibiotic therapy should be targeted to these pathogens. The presence of an abscess should raise concern for anaerobes. The most appropriate choice of the above would be ampicillin-sulbactam. Coverage for methicillin-resistant Staphylococcus aureus could be considered if the patient has risk factors or is not improving, but vancomycin alone would be inappropriate monotherapy. Piperacillin-tazobactam would provide excessively broad coverage as this patient does not have risk factors for a pseudomonal or other resistant Gram-negative infection. Agents with better central nervous system penetration (vancomycin, ceftriaxone and metronidazole) should be started if there is concern for intracranial extension.
QUESTION #3
For orbital cellulitis, surgical intervention should be considered for all the following EXCEPT?
- Abscess diameter >5 mm
- Poor response despite appropriate antibiotics for 24-48 hours
- Visual changes on physical examination
- Concerns for intracranial extension
ANSWER #3
A. Abscess diameter >5 mm
Indications for surgery include large abscess >10 mm in diameter, vision changes or any threatened visual loss, failure of improvement with appropriate antibiotic treatment after 24-48 hours, or present intracranial extension. For this reason, it is important to involve otolaryngology and ophthalmology early in the patient’s course of care.
CLINICAL COURSE
Ampicillin-sulbactam was started. Ophthalmology, otolaryngology and infectious diseases were consulted. Due to the presence of the subperiosteal abscess and the inability of the CT scan of the referring facility to evaluate thoroughly for intracranial extension, an MRI of the brain (with/without contrast) was obtained on hospital day 1. Evaluation showed the known subperiosteal abscess with proptosis but additionally demonstrated leptomeningeal enhancement adjacent to the frontal lobes concerning for intracranial extension.
Antibiotics were switched to vancomycin, ceftriaxone and metronidazole for better penetration of the central nervous system. Cerebrospinal fluid from a lumbar puncture performed on hospital day 2 did not show evidence of meningitis. Due to persistent fever and imaging findings, the patient was taken to the operating room on hospital day 2 with otolaryngology and underwent functional endoscopic sinus surgery (FESS) with bilateral maxillary antrostomies and drainage of the subperiosteal abscess of the right orbit. Intraoperative cultures grew Streptococcus pyogenes (group A Streptococcus), and the patient was switched back to ampicillin-sulbactam and ultimately transitioned to amoxicillin-clavulanate. Of note, this antibiotic was selected as it would also provide coverage for anaerobes that may have been present within the abscess but not growing in culture. The patient completed 21 days of treatment with complete resolution.
Sources:
- DynaMed. Orbital cellulitis. EBSCO Information Services. Accessed February 2, 2023. https://www.dynamed.com/condition/orbital-cellulitis
- Milo RB. Preseptal cellulitis versus orbital cellulitis: a pediatric case. Adv Emerg Nurs J. 2022;44(3):199-205. PMID: 35900239. doi:10.1097/TME.0000000000000416
- Nageswaran S, Woods CR, Benjamin DK Jr, Givner LB, Shetty AK. Orbital cellulitis in children. Pediatr Infect Dis J. 2006;25(8):695-9. PMID: 35900239. doi:10.1097/01.inf.0000227820.36036.f1
- Wong SJ, Levi J. Management of pediatric orbital cellulitis: a systematic review. Int J Pediatr Otorhinolaryngol. 2018;110:123-129. PMID: 29859573. doi:10.1016/j.ijporl.2018.05.006.
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care - read the February issue of The Link.
