An Increase in Invasive Group A Streptococcus Infections
Outbreaks, Alerts and Hot Topics - February 2023
Column Author and Editor: Chris Day, MD | Pediatric Infectious Diseases; Director, Transplant Infectious Disease Services; Medical Director, Travel Medicine; Assistant Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
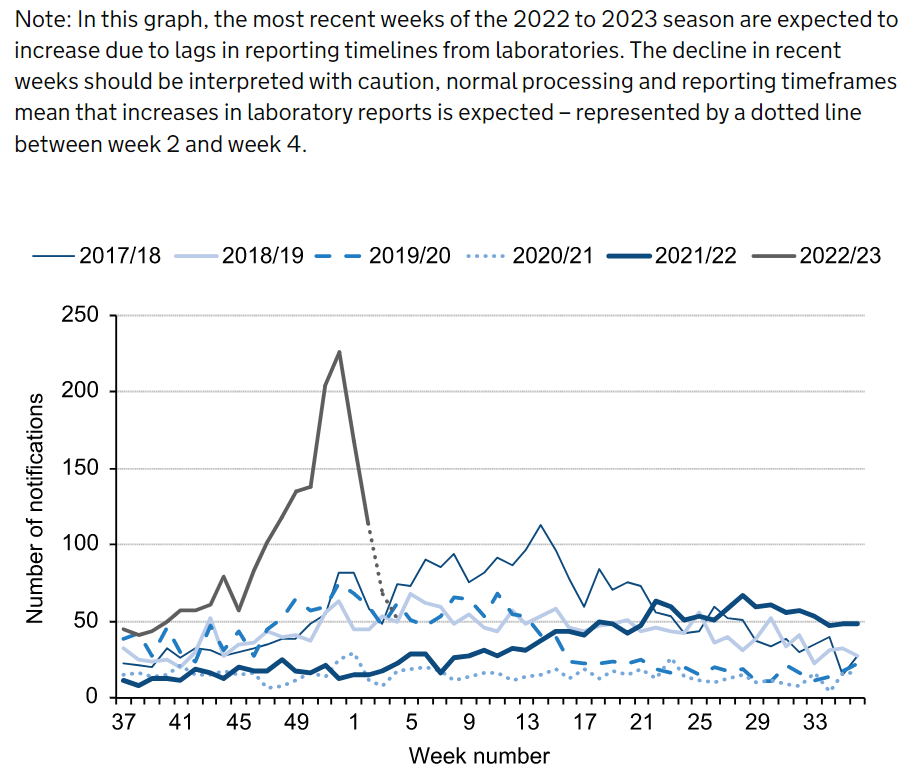
The Centers for Disease Control and Prevention is currently investigating an increase in invasive group A streptococcal (iGAS) infections in children in the U.S. The incidence of iGAS infection has been low over the past several years, likely related to measures taken to prevent transmission of SARS-COV-2. Although recent levels of iGAS disease in the U.S. are similar to those seen prior to the pandemic, they appear to be occurring earlier in the respiratory season than has been typical.1 The World Health Organization is also reporting concerns of increased iGAS infections in children in at least five European countries (France, Ireland, the Netherlands, Sweden and the United Kingdom).2 In England specifically, there has been an abrupt increase over usual in reports of iGAS (Figure) including 29 deaths reported in children under age 15 and 235 deaths overall (attributed deaths occurred within seven days of a laboratory report of iGAS infection and may underestimate attributable mortality).3
Figure: Weekly laboratory notifications of invasive GAS, England, by season, 2017 to 2018 onwards (weeks 37 to 4).4
Invasive infection is defined by the isolation of group A Streptococcus from a normally sterile body site. Depending on the site of invasion, iGAS can include cellulitis, necrotizing fasciitis, bacterial pneumonia, osteomyelitis, septic arthritis or lymphadenitis. Streptococcal toxic shock syndrome (STSS) can occur in conjunction with any of these invasive infections but is particularly associated with skin and soft tissue infections (80% of patients with STSS) and with progression to necrotizing fasciitis.5
The current situation with iGAS in North America and Europe may be secondary in part to an early respiratory viral season. Many iGAS infections likely follow respiratory viral infections and are known to be sequelae of chickenpox infections. Immunization with varicella, influenza and COVID-19 vaccines likely helps to reduce the risk of these infections.1-3
STSS is diagnosed in anyone meeting the clinical case definition:
“An illness associated with invasive or noninvasive group A strep infection with the following clinical manifestations:
- Hypotension defined by a systolic blood pressure less than or equal to 90 mm Hg for adults or less than the fifth percentile by age for children aged less than 16 years.
- Multi-organ involvement characterized by two or more of the following:
-
- Renal impairment: Creatinine greater than or equal to 2 mg/dL (greater than or equal to 177 µmol/L) for adults or greater than or equal to twice the upper limit of normal for age. In patients with preexisting renal disease, a greater than twofold elevation over the baseline level.
- Coagulopathy: Platelets less than or equal to 100,000/mm3 (less than or equal to 100 x 106/L) or disseminated intravascular coagulation, defined by prolonged clotting times, low fibrinogen level, and the presence of fibrin degradation products.
- Liver involvement: Alanine aminotransferase, aspartate aminotransferase, or total bilirubin levels greater than or equal to twice the upper limit of normal for the patient’s age. In patients with preexisting liver disease, a greater than twofold increase over the baseline level.
- Acute respiratory distress syndrome: Defined by acute onset of diffuse pulmonary infiltrates and hypoxemia in the absence of cardiac failure or by evidence of diffuse capillary leak manifested by acute onset of generalized edema, or pleural or peritoneal effusions with hypoalbuminemia.
- A generalized erythematous macular rash that may desquamate.
-
- Soft-tissue necrosis, including necrotizing fasciitis or myositis, or gangrene.”6
Treatment for STSS requires hospitalization and appropriate fluid resuscitation. A broad antibiotic regimen may be required initially before group A strep has been isolated, but once iGAS is confirmed as the cause of the shock, penicillin (or ampicillin) and clindamycin (the latter to reduce toxin production by acting directly on the bacterial ribosome) can be used as definitive therapy.6 The hallmark of necrotizing fasciitis is pain that is out of proportion to the signs visible on exam. Treatment of necrotizing fasciitis also requires hospitalization as well as emergent fasciotomy and surgical debridement.7
References:
- National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases. Centers for Disease Control and Prevention. Increase in invasive group A strep infections, 2022-2023. Reviewed February 2, 2023. Accessed February 7, 2023. https://www.cdc.gov/groupastrep/igas-infections-investigation.html
- World Health Organization. Disease outbreak news; increased incidence of scarlet fever and invasive group A Streptococcus infection – multi-country. December 15, 2022. Accessed February 7, 2023. https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON429
- UK Health Security Agency. Group A streptococcal infections: eighth update on seasonal activity in England. Updated February 3, 2023. Accessed February 7, 2023. https://www.gov.uk/government/publications/group-a-streptococcal-infections-activity-during-the-2022-to-2023-season/group-a-streptococcal-infections-eighth-update-on-seasonal-activity-in-england
- Source for figure: UK Health Security Agency. Group A streptococcal infections: eighth update on seasonal activity in England. Updated February 3, 2023. Accessed February 7, 2023. https://www.gov.uk/government/publications/group-a-streptococcal-infections-activity-during-the-2022-to-2023-season/group-a-streptococcal-infections-eighth-update-on-seasonal-activity-in-england (Free to re-use per crown copyright under Open Government License)
- Stevens DL. Streptococcal toxic-shock syndrome: spectrum of disease, pathogenesis, and new concepts in treatment. Emerg Infect Dis. 1995;1(3):69-78.
- National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases. Centers for Disease Control and Prevention. Streptococcal toxic shock syndrome. Reviewed June 27, 2022. Accessed February 7, 2023. https://www.cdc.gov/groupastrep/diseases-hcp/Streptococcal-Toxic-Shock-Syndrome.html#:~:text=Streptococcal%20toxic%20shock%20syndrome%20(STSS,organ%20failure%2C%20and%20frequently%20death
- National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases. Centers for Disease Control and Prevention. Type II necrotizing fasciitis. Reviewed June 27, 2022. Accessed February 7, 2023. https://www.cdc.gov/groupastrep/diseases-hcp/necrotizing-fasciitis.html
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care - read the February issue of The Link.
