Evaluating Growth Failure
A Pediatric Guide from Children’s Mercy Kansas City
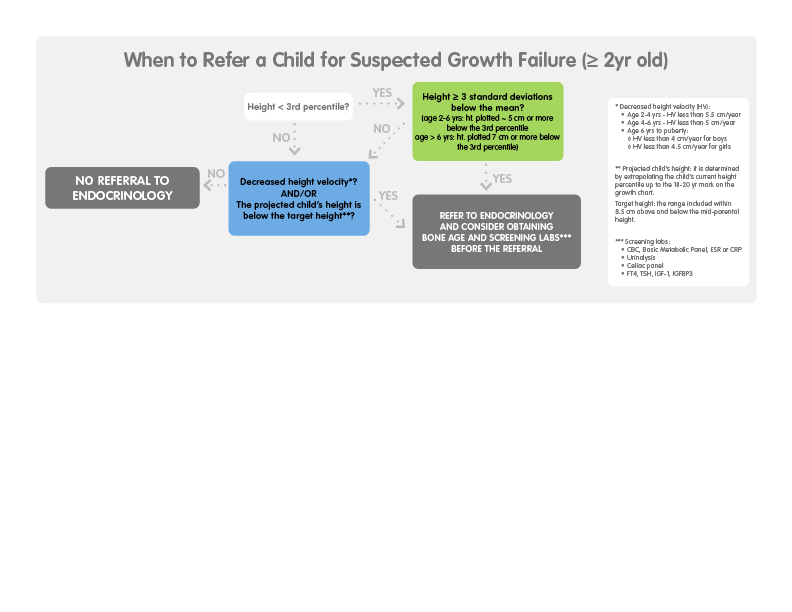
Who should be referred to the endocrinologist for further evaluation of suspected growth failure?
The decision to refer a child with short stature usually depends on the answers given to these three questions:
- How short is the child?
- Is the child’s height velocity (HV) impaired?
- Is the child’s height/growth within the range for the family?
How short is the child?
- If the child’s height is above – 2SD (above the 3rd percentile), he has a normal stature. Thus, he generally does not require further evaluation, unless his statural growth curve crosses height percentiles downward, the child has dysmorphic features, or evidence of underlying systemic disease, or if the child’s height percentile is well below the target height.
- If the child’s height is below – 2SD (below the 3rd percentile), he has short stature. If his height is above – 3SD (within 5 to 7 cm below the 3rd percentile), an initial evaluation of the child’s height velocity (see below) should be performed in the primary care setting. A referral to the endocrinologist is appropriate if the height velocity is slow for age and gender.
- If the child’s height is below – 3SD (it is plotted ~5 cm or more below the 3rd percentile between age 2 to 6 years, and ~7 cm or more below the 3rd percentile beyond age 6), the child has severe short stature. Since there is a high likelihood of a pathologic cause of short stature, the child should be referred to the endocrinologist.
Is the child’s height velocity impaired?
Determination of the child’s height velocity requires repeated measurements of the height, which should be measured with an interval of at least 6 months between measurements.
For children 2 years and older, growth failure is likely if the child is growing more slowly than the following rates:
- Age 2-4 years – HV less than 5.5 cm/year (< 2.2 inches/year)
- Age 4-6 years – HV less than 5 cm/year (< 2 inches/year)
- Age 6 years to puberty:
- HV less than 4 cm/year for boys (< 1.6 inches/year)
- HV less than 4.5 cm/year for girls (< 1.8 inches/year)
Is the child’s height/growth within the range for the family?
The next step is to determine the height range expected for that child, based on the biologic family’s height (child’s genetic height potential) and compare it with the child’s current growth trajectory.
An estimate of a child’s genetic height potential can be obtained by calculation of the mid-parental height, which is based upon the heights of both parents and adjusted for the sex of the child (see formula). For both girls and boys, the range included within 8.5 cm above and below the mid-parental height represents what is called target height (3rd to 97th percentiles for anticipated adult height).
The projected height for a child is determined by extrapolating the child’s current height curve/channel up to the 18- to 20-year mark on the growth chart. If the child’s projected height is within the target height, then the child’s height is within the expected range for the family. This child probably has familial short stature, which is considered a variant of normal growth, and thus he does not need to be referred to a specialist (unless his mid-parental height is significantly below the normal range).
If the child’s projected height is below the target height, then the child can be considered abnormally short for his or her family, and thus may need to be referred for further evaluation.
Is an initial diagnostic evaluation in the primary care setting needed?
The difference between short stature and growth failure
By definition, ~2% of the pediatric population is short; however, the majority of these children do not have growth failure. Short stature is defined as a length or height below the 2.3rd percentile for age and gender (for approximation, we often used the 3rd percentile, since the 2.3rd percentile is not included in the most-used growth charts). Often, but not always, short stature and growth failure coexist in the same child. An exception may be a child who may have a normal variant of growth, such as familial short stature and/or constitutional growth delay.
On the other hand, a child may have growth failure without short stature (for example, height percentile for age falling from 90th percentile to 50th percentile after age 3). Evidence indicates that a child with short stature without suspicious signs and/or symptoms of an underlying pathology (abnormal findings on history, review of systems, or physical exam), and with a normal growth velocity very rarely has growth failure (only ~2% of the time). The likelihood of experiencing growth failure is higher in children with more severe short stature (e.g., whose height is significantly below the 3rd percentile) and/or reduced growth velocity.
Once the primary care physician has decided to refer the child to an endocrinologist for suspected growth failure, the primary care physician may want to consider obtaining an initial diagnostic work-up.
Bone age determination
Bone age is typically determined from a radiograph of the left hand. The method most commonly used to determine the bone age is based on using the Greulich and Pyle Atlas. The bone age determination informs estimates of the child’s growth potential and likely adult height.
A delayed bone age does not necessarily imply growth failure; it can be consistent with constitutional delay of growth and puberty (CDGP), which is considered a normal variant of growth. However, significantly delayed bone age is also seen in many types of growth failure, including nutritional deficiency, underlying systemic disease (such as inflammatory bowel disease), growth hormone deficiency and hypothyroidism.
A normal bone age is consistent with several diagnostic possibilities. In a child with short parents, a normal bone age supports the diagnosis of familial short stature. However, a normal bone age may also be seen in girls with Turner syndrome.
Laboratory studies
Screening laboratory tests may be considered by the primary care physician in case of impaired growth velocity (see above) and if the history or physical examination raise suspicion for an underlying pathology.
Useful screening tests:
- Complete blood count (CBC) and erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)
- Electrolytes, creatinine, bicarbonate, calcium, phosphate, alkaline phosphatase, albumin
- Celiac serologies (e.g., tissue transglutaminase [tTG] immunoglobulin A [IgA] and total IgA)
- Free T4, TSH, IGF-1, IGFBP3
Suspicious findings in the history
- Systemic symptoms such as sluggishness, lethargy, cold intolerance, constipation
- Gastrointestinal symptoms, including decreased appetite, abdominal pain, diarrhea, and rectal bleeding
- Pulmonary symptoms, including severe asthma
- Recurrent infections
- Arthralgia or arthritis
- Medications – Prolonged or frequent use of glucocorticoids (including inhaled glucocorticoids) or use of stimulants for attention deficit hyperactivity disorder
Suspicious findings in the physical examination
- Weight loss, poor weight gain, underweight for height, and delayed puberty
- Developmental delay/learning disabilities
- Facial dysmorphisms
- Hypertelorism, downward eye slant, low-set ears
- Prominent forehead, Midface hypoplasia, frontal bossing, triangular face, downturned corners of the mouth
- Midline defects
- Webbed neck
Referral instructions
Calculating mid-parental height
Children usually reach an adult height that is within 2 standard deviations (~8.5 cm) above and below their mid-parental height. This estimated range is known as the “target height.”
The mid-parental height is based on the heights of both parents and adjusted for the sex of the child:
- Girls: 13 cm (or 5 inches) is subtracted from the father’s height and averaged with the mother’s height.
- Boys: 13 cm (or 5 inches) is added to the mother’s height and averaged with the father’s height.
Nutritional deficits, organic diseases, or endocrine disorders may prevent a child from attaining the expected adult height.
Refer concerns regarding abnormal growth failure or short stature to pediatric endocrinology for further evaluation.
At Children’s Mercy, patients have access to an established, experienced team of more than 20 pediatric endocrinologists and nearly 100 staff members who specialize in endocrine disorders.
Make a referral
Select “Endocrine” from the list of specialties and “FTT/Short stature/Growth Failure” under “Reasons for Consultation.”
All new referral requests are processed within 48 hours. Two phone attempts to contact the family and a final notification to the family to schedule will be made. For assistance, call the Contact Center at (816) 234-3700 or toll-free at (800) 800-7300. The Contact Center can provide additional information regarding any supporting documentation needed for the referral.
For urgent requests to speak to a specialist, please call and ask to speak with the on-call pediatric subspecialist at 1 (800) GO-MERCY / (800) 466-3729.
These instructions are provided for informational purposes only. The choice of provider referral is at your discretion.
Additional resources
- Sisley S, Vargas Trujillo M, Khoury J, Backelijauw P. Low Incidence of Pathology Detection and High Cost of Screening in the Evaluation of Asymptomatic Short Children. J Pediatr. 2013; 163: 1045-1051.
- Pinhas-Amiel O, De Luca F, Allen DB. Chapter 2: Normal Growth and Growth Disorders. In Pediatric Endocrinology: Essentials for Practice, McGraw-Hill, 3rd edition, in press.
- Rogol AD, Hayden G. Etiologies and Early Diagnosis of Short Stature and Growth Failure in Children and Adolescents. J Pediatr. 2014; 164: S1-14.
- Savage MO, Backeljauw P, Calzada R, et al. Early Detection, Referral, Investigation, and Diagnosis of Children with Growth Disorders. Horm res Paediatr. 2016; 85: 325-332.
- Oostdijk W, Grote FK, de Muinck Keizer-Schrama S. Diagnostic Approach in Children with Short Stature. Horm Res. 2009; 72: 206-217.
- Richmond EJ, Rogol AD. Diagnostic Approach to Children and Adolescents with Short Stature. UpToDate, last updated in Jan 2020.
- 2007 WHO Growth Charts; 2000 CDC Growth Charts.
