Abnormal Thyroid
A Pediatric Guide from Children’s Mercy
When should thyroid function tests be ordered?
Which TFTs should be ordered?
TSH is the single most sensitive test used to diagnose primary hypothyroidism (high TSH) or hyperthyroidism (low TSH). In these situations, free T4 (FT4) is low or high respectively; when this occurs, the diagnosis of an overt thyroid illness is very likely, and the child will need to be referred to a pediatric endocrinologist.
- It is important to evaluate TSH levels in the context of age, since TSH normal ranges are higher in infancy when compared to older children.
- A TSH measurement alone is not accurate in diagnosing central hypothyroidism, since TSH may be normal or low-normal while FT4 is typically below the normal range.
- Measuring FT4 without TSH may lead to an incorrect diagnosis of a thyroid disease. For example, a non-thyroidal illness, the use of drugs like valproate, carbamazepine and phenobarbital, or the inaccuracy of some free T4 immunoassays, can result in an under-estimation of FT4.
Thus, in case there is a suspicion of a thyroid disease, obtain both TSH and FT4.
Between 25-50% of the referrals to a pediatric endocrinology clinic are related to abnormal thyroid function tests (TFTs). The majority of these abnormal TFTs are not associated with a true thyroid problem, especially when these tests are ordered in the absence of any signs or symptoms suggestive of a thyroid disease.
We recommend TFTs be ordered in any of these situations:
- Any child with an enlarged thyroid (goiter) on physical examination
- Signs or symptoms of hypothyroidism:
- New onset or worsened fatigue
- Declining statural growth rate
- Constipation, dry skin, cold intolerance
- Declining school performance
- Menstrual abnormalities
- Signs or symptoms of hyperthyroidism:
- Unexplained weight loss
- Hyperactivity, emotionality, depression-like behavior
- Palpitations, tachycardia
- Heat intolerance
- Declining school performance
- Menstrual abnormalities
Many of the symptoms of hypothyroidism are non-specific. However, the likelihood to be secondary to a thyroid disease increases in the presence of the following risk factors:
- Down or Turner syndrome
- Previous diagnosis of an autoimmune disorder, such as type 1 diabetes or celiac disease
- History of a thyroid disease in first-degree relatives
- Drugs, like lithium and amiodarone
- Head and neck radiation
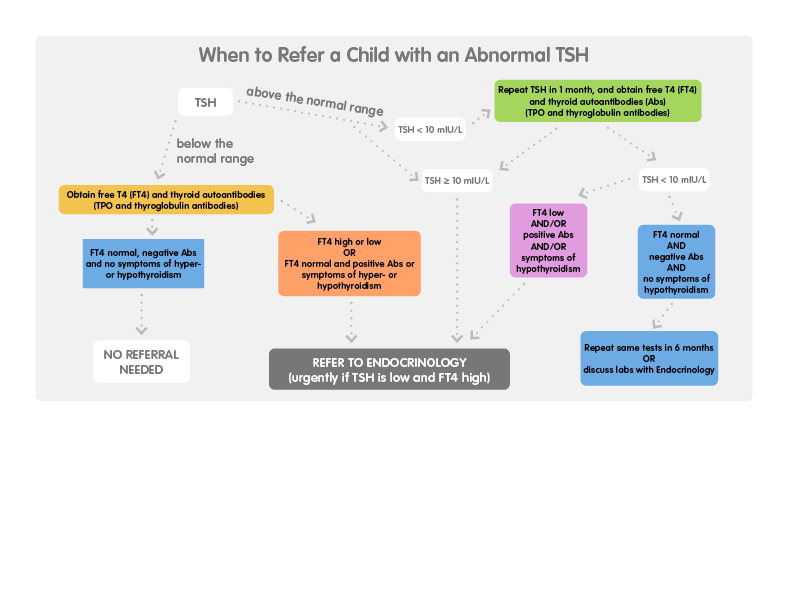
What should be done if the TSH is abnormal?
High TSH
A high serum level of TSH is not an uncommon finding. Studies in large pediatric populations have identified ~4% of children with high TSH.
TSH levels above 10 mIU/L are typically associated with positive thyroid autoantibodies and/or low FT4. Thus, they need to be referred to a pediatric endocrinologist.
However, TSH values are often only slightly above the age-appropriate range (< 10 mIU/L) and are typically found in asymptomatic children with normal FT4 (“subclinical hypothyroidism”). Evidence indicates that children with subclinical hypothyroidism experience none of the typical features of overt hypothyroidism. In addition, treating children with subclinical hypothyroidism has shown no benefit.
- Once a slightly high TSH is repeated, more than 70% of the time it is found to be normal.
- If repeat TFTs confirm a slightly high TSH, normal FT4, and negative thyroid autoantibodies, it is appropriate to repeat them one more time in ~6 months, or review them with a pediatric endocrinologist.
- An exception to this guideline is a slightly elevated TSH in an infant younger than 1 year of age. Given the child’s higher risk to progress to overt hypothyroidism, we recommend referral to a pediatric endocrinologist before repeating the TFTs.
An isolated mild increase of TSH (associated with normal FT4), is a relatively common finding in overweight or obese children (7% to 23% in two studies). However, it seems to represent an adaptive response to obesity rather than a cause of it. Indeed, TSH usually normalizes after weight loss. The recently published Endocrine Society Clinical Practice Guidelines discourage from obtaining screening TFTs in children with obesity, unless excessive weight gain is associated with declining statural growth.
Low TSH
A low TSH is more rarely detected than a high TSH. It is typically found in children with overt hyperthyroidism when it is usually very low (< 0.01 mIU/L) and associated with high FT4 and/or total T3.
A slightly low TSH, along with a normal FT4 (“subclinical hyperthyroidism”) is much less common in children than in adults. Prospective studies have shown that only ~1% of patients with subclinical hyperthyroidism progress to overt hyperthyroidism in a 5-year period, with the rest of them having a normalized or persistently slightly low TSH on repeat testing.
Thus, in an asymptomatic child with a slightly low TSH, normal FT4 and negative thyroid autoantibodies, there is no indication for a referral to a pediatric endocrinologist.
Biotin supplementation is known to cause falsely low TSH by interfering with biotin-based TSH immunoassays. Less often, it can cause falsely high free T4. Biotin is often used to promote healthy hair and nails, and in a number of metabolic disorders. If a child is taking high doses of biotin (> 100 mg/day), this supplement should be discontinued at least 2 days before obtaining TSH and free T4.
Referral instructions
Refer concerns regarding abnormal TSH or thyroid disease to pediatric endocrinology for further evaluation.
At Children’s Mercy, patients have access to an established, experienced team of more than 20 pediatric endocrinologists and nearly 100 staff members who specialize in endocrine disorders.
Make a referral
Select “Endocrine” from the list of specialties and “Hyperthyroidism” or “Hypothyroidism” under “Reasons for Consultation.”
All new referral requests are processed within 48 hours. Two phone attempts to contact the family and a final notification to the family to schedule will be made. For assistance, call the Contact Center at (816) 234-3700 or toll-free at (800) 800-7300. The Contact Center can provide additional information regarding any supporting documentation needed for the referral.
For urgent requests to speak to a specialist, please call and ask to speak with the on-call pediatric subspecialist at 1 (800) GO-MERCY / (800) 466-3729.
These instructions are provided for informational purposes only. The choice of provider referral is at your discretion.
Additional resources
- Lazar L, Ben-David Frumkin R, Battat E, et al. Natural History of Thyroid Function Tests Over 5 Years in a Large Pediatric Cohort. J Clin Endocrinol Metabol. 2009; 94: 1678-1682.
- Schushan I, Lazar L, Amitai N, Meyerovitch J. Thyroid Function in Healthy Infants During the First Year of Life. J Pediatr. 2016; 170: 120-125.
- Gammons S, Presley BK, White PC. Referrals for Elevated Thyroid Stimulating Hormone to Pediatric Endocrinologists. J Endocr Soc. 2019; 3: 2032-2040.
- Wasniewska M, Aversa T, Salerno M, et al. Five-year Prospective Evaluation of Thyroid Function in Girls with Subclinical Mild Hypothyroidism of Different Etiology. Eur J Endocrinol. 2015; 173: 801-808.
- Vigone MC, Capalbo D, Weber G, et al. Mild Hypothyroidism in Childhood: Who, When, and How Should be Treated? J Endocr Soc. 2017; 2: 1024-1039.
- Vadiveloo T, Donnan P, Cochrane L, et al. The Thyroid Epidemiology, Audit, and Research Study (TEARS): The Natural History of Endogenous Subclinical Hyperthyroidism. J Clin Endocrinol Metabol. 2011; 96 (5):1344-51.
