Abnormal Menstrual Patterns
A Pediatric Guide from Children’s Mercy Kansas City
Evaluating abnormal menstrual patterns
According to the American College of Obstetricians and Gynecologists, a number of medical conditions can cause abnormal uterine bleeding, characterized by unpredictable timing and a variable amount of flow. Although a long interval between cycles is common in adolescence for the first 2 years after menarche, it is uncommon for girls and adolescents to remain amenorrheic for more than 3 months or 90 days (the 95th percentile for cycle length). Girls and adolescents with more than 3 months between periods or those that remain otherwise irregular 2 years after menarche, should be evaluated for underlying causes.
PCOS
What is PCOS?
PCOS is a hormonal condition that affects 6-15% of women of reproductive age. PCOS develops in genetically predisposed females where the severity of clinical expression is compounded by environmental, nutritional and lifestyle factors. The genetic predisposition mainly affects ovarian function manifesting in a tendency toward ovulation dysregulation and hormonal imbalance which favors androgen production. Short- and long-term consequences of menstrual dysfunction and hormonal imbalance may include hirsutism and severe acne, depression and anxiety, insulin resistance, weight gain and diabetes, non-alcoholic fatty liver disease, heart disease, endometrial cancer, infertility and miscarriages.
When should patients with possible PCOS be referred?
Strongly consider a diagnosis of PCOS if there is menstrual irregularity coupled with biochemical or clinical hyperandrogenism (hirsutism/severe acne).
- Screening total testosterone > 40 ng/dL
- Hirsutism (hair on upper lip, chin, chest, lower abdomen and upper back)
- May use modified Ferriman-Gallwey Score (see chart)
- Menstrual irregularity as defined here
The MAPP clinic offers same-day diagnostic services for those with presumed PCOS such as ultrasound and oral glucose tolerance test. The clinic also offers professional nutritional counseling. Should the adolescent also have questions and concerns regarding psychological or reproductive health issues, Adolescent Medicine specialists are present for confidential discussion.
1. Perform history and clinical evaluation
Family history:
- Ask about irregular menstrual patterns
- Thyroid conditions
- PCOS
- Diabetes
Personal history:
- Changes in weight
- Change in eating/exercise patterns
- Change in medications
- Pregnancy risk
- History of polyuria/polydipsia
- Changes in vision
- Headaches
Physical exam:
- Look for or make note of male pattern hair growth (upper lip, chin, chest, lower abdomen and upper back) (see boxes on PCOS and hirsutism)
- Prominent acne
- Signs of autoimmune disease (vitiligo)
- Signs of insulin resistance (acanthosis)
- Violaceous stretch marks
2. Initial laboratory evaluation
- Rule out pregnancy
- TSH
- Total and free testosterone
- Prolactin
- LH, FSH
Further potential laboratory evaluation (can be done in Endocrine Clinic):
- Hba1c
- DHEAS, androstenedione, 17-hydroxyprogesterone
3. When should patients be referred to Children’s Mercy Endocrinology?
- If menstrual cycles are abnormal and there is physician or NP/PA concern for an endocrine condition. No prior labs required.
- If any of the above hormonal labs are out of range, a referral for that specific concern can be made (unless the patient tests positive for pregnancy).
- If there is concern for PCOS, refer directly to the Multispecialty Adolescent PCOS Program (MAPP).
Referral instructions
Refer concerns regarding abnormal menstrual cycles, suspicion of PCOS or hirsutism, to pediatric endocrinology for further evaluation.
At Children’s Mercy, patients have access to an established, experienced team of more than 20 pediatric endocrinologists and nearly 100 staff members who specialize in endocrine disorders. Our Multispecialty Adolescent PCOS Program helps girls and teens manage the symptoms of PCOS, including irregular menstrual cycles and elevated levels of androgens in the female body.
Make a referral
Select “Endocrine” from the list of specialties and “PCOS” under “Reasons for Consultation.”
All new referral requests are processed within 48 hours. Two phone attempts to contact the family and a final notification to the family to schedule will be made. For assistance, call the Contact Center at (816) 234-3700 or toll-free at (800) 800-7300. The Contact Center can provide additional information regarding any supporting documentation needed for the referral.
For urgent requests to speak to a specialist, please call and ask to speak with the on-call pediatric subspecialist at 1 (800) GO-MERCY / (800) 466-3729.
Excess body hair
What is on the differential for excess body hair?
- Hypertrichosis
- Medication-induced side effect
- Idiopathic/genetic
- Hirsutism related to hyperandrogenemia
- PCOS
- CAH
- Androgen-secreting tumors
- Idiopathic hirsutism
What is hypertrichosis?
Hypertrichosis is excessive hair growth above normal for age, sex and race and can be seen on all areas of the body, not only androgen-dependent regions. Contrary to hirsutism, the hair in hypertrichosis is less coarse.
What is hirsutism?
Hirsutism is excessive terminal hair (longer, pigmented, coarse) in androgen-dependent areas of the female body. This includes areas such as the upper lip, chin, chest, lower abdomen and upper back. A detailed method for determining degrees of hirsutism is the modified Ferriman Gallwey Score (mFGS). A score of 4-6 suggests hirsutism.
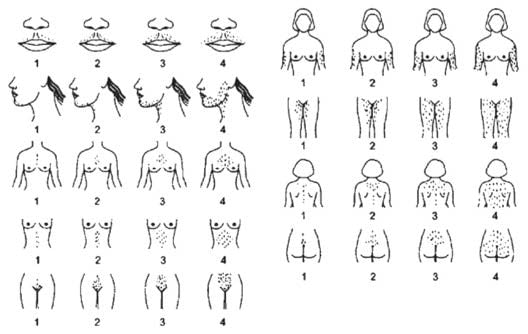
When should patients with hirsutism be referred?
Refer to pediatric endocrinology if there is a physical exam concerning for hirsutism (hair on upper lip, chin, chest, lower abdomen or upper back). Modified FGS score is not needed for referral.
These instructions are provided for informational purposes only. The choice of provider referral is at your discretion.
Additional resources
- Witchel SF, Oberfield S, Rosenfield RL, et al. The Diagnosis of Polycystic Ovary Syndrome during Adolescence [published online ahead of print, 2015 Apr 1]. Horm Res Paediatr. 2015;doi:10.1159/000375530.
- Teede HJ, Misso ML, Costello MF, et al. Recommendations from the International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome. Fertil Steril. 2018;110(3):364-379. doi:10.1016/j.fertnstert.2018.05.004.
- Escobar-Morreale HF, Carmina E, Dewailly D, et al. Epidemiology, Diagnosis and Management of Hirsutism: A Consensus Statement by the Androgen Excess and Polycystic Ovary Syndrome Society [published correction appears in Hum Reprod Update. 2013 Mar Apr;19(2):207]. Hum Reprod Update. 2012;18(2):146-170. doi:10.1093/humupd/dmr042.
