Drowning: What's the Diagnosis?
Visual Diagnosis - June 2023
Column Author and Editor: Joe Julian, MD, MPHTM | Hospitalist, Internal Medicine-Pediatrics; Clinical Associate Professor, Internal Medicine & Pediatrics
THE CASE
A 10-month-old male is evaluated after drowning event at neighborhood pool. He was in the baby pool with several adults sitting nearby. One adult noticed that patient was missing and found him facedown in the water. The estimated down time was 20 seconds. He was immediately responsive and breathing. No chest compressions or rescue breaths were required. He had an episode of perioral cyanosis and decreased activity. There is no family history of lung disease, cardiac arrhythmias or sudden unexplained cardiac death.
Vital signs notable for a heart rate of 155, a respiratory rate of 43, and pulse oximetry of 100% on room air. Examination is notable for age-appropriate activity, a normal work of breathing, crackles at the left lung base, a heart rate that is regular without rhythm, and well-perfused skin without cyanosis.
QUESTIONS
Question #1 – What is this patient’s diagnosis?
- Drowning
- Near drowning
- Wet drowning
- Dry drowning
A. Drowning is the correct answer. “Non-fatal drowning” would also be acceptable. Other terminology (such as near, wet and dry drowning) is now outdated and considered inappropriate terminology that can cause confusion and limit correct disposition of patient. Drowning is respiratory impairment related to submersion in liquid and can cause respiratory compromise at the time of the event and up to eight hours later.
Question #2 - Which of the following is the next best step in evaluation?
- No further evaluation
- Two-view chest radiography
- Basic metabolic panel (BMP)
- Electrocardiogram (ECG)
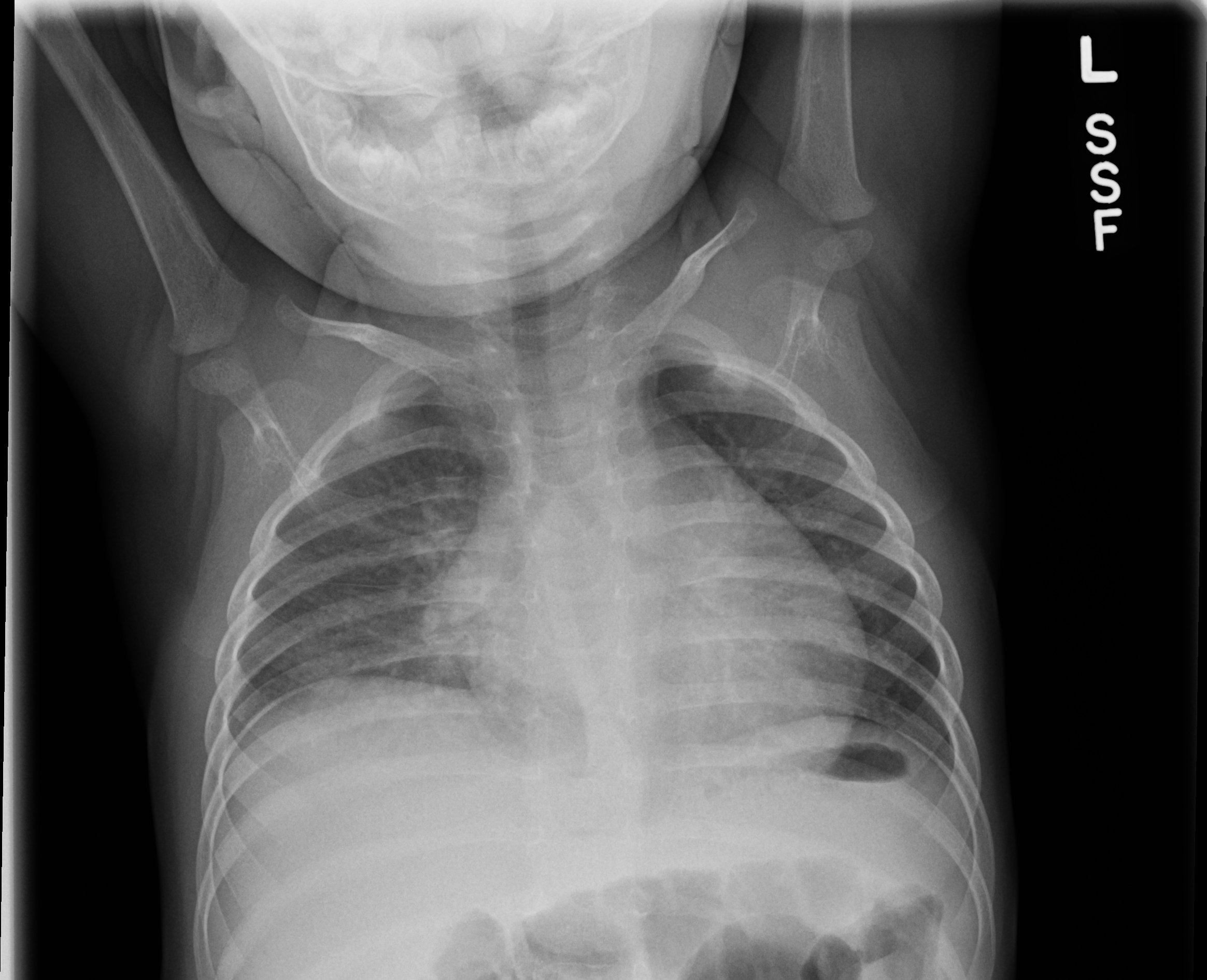
There are two acceptable answers here – A. No further evaluation and B. Two-view chest radiography. This patient is already noted to have crackles on examination and presumptively has some degree of pulmonary edema. If the examiner is clinically uncertain about the presence of a pulmonary edema, chest radiography may be useful. However, it is unclear how chest radiography fits into disposition of a patient who has sustained drowning. Several tertiary databases do recommend imaging as part of evaluation. Abnormal chest radiography generally shows improvement within 24 hours.
A BMP would not be expected to show any significantly abnormal results. Derangement of sodium values, in the rare instance it does occur and requires treatment, occurs in the setting of aspiration of large amounts of water.
An ECG would be useful in the setting of drowning if the occurrence is unexplained (such as in a person who is swimming capable without clear inciting event) or if there is a family history of sudden cardiac death. Given the lack of family history and clear inciting event consistent with patient’s development, ECG is not a high-yield test.
This patient received chest radiography which is shown below:
Question #3 - Which of the following is the next best step in treatment?
- Supplemental oxygen
- Intravenous fluids
- Steroids and antibiotics
- No further treatment
D. No further treatment is the correct answer. This patient is neither hypoxemic nor volume depleted and does not require supplemental oxygen or IV fluids. Steroids and antibiotics are not indicated patients with no to moderate symptoms. There may be a role for prophylactic antibiotics if the patient drowned in contaminated water (something with high sewage content).
Question #4 - Which of the following is the best choice for patient disposition?
- Discharge home now with follow-up
- Admit to floor for observation
- Observe for eight hours then discharge
- Admit to intensive care unit
There are two acceptable answers here – B. Admit to floor for observation and C. Observe for eight hours then discharge. Most data on patients who have drowned involves those with more serious presentations. There is no consensus on the disposition of patients who are asymptomatic or have mild to moderate symptoms. In this patient, abnormal lung sounds and some mild tachypnea persisted several hours after the event. These symptoms, combined with the chest radiography and evening admission, prompted shared decision-making for overnight observation in the hospital.
If this patient had presented earlier in the day and had a normal examination and vital signs at eight hours post-drowning, it would be reasonable to consider discharge home given the very low risk of further decompensation. Given the dearth of clear evidence, any clinical concern should prompt a longer period of observation.
This patient does not require intensive level of care (which would be indicated for non-invasive or mechanical ventilation). Discharging the patient immediately with an abnormal pulmonary examination prior to six to eight hours of observation increases the risk of clinical worsening requiring intervention while at home.
CASE RESOLUTION
The patient was observed overnight and did not require supplemental oxygen. His vital signs remained within age-appropriate limits and he was discharged the following morning.
DROWNING PREVENTION TIPS
- Prevention is key when it comes to drowning.
- Swim lessons for parents and toddlers should be encouraged.
- An adult (“water watcher”) who is 100% dedicated to water supervision should be assigned.
More information from the American Academy of Pediatrics is available here.
LITERATURE
- Bierens J, Abelairas-Gomez C, Barcala Furelos R, et al. Resuscitation and emergency care in drowning: a scoping review. Resuscitation. 2021;162:205-217.
- Brenna CE, Hong TKF, Wang VJ. Predictors of safe discharge for pediatric drowning patients in the emergency department. Am J Emerg Med. 2018;36(9):1619-1623.
- Cantu RM, Pruit CM, Samuy N, Wu CL. Predictors of emergency department discharge following pediatric drowning. Am J Emerg Med. 2018;36(3):446-449.
- Cohen N, Capua T, Lahat S, Glatstein M, Sadot E, Rimon A. Predictors for hospital admission of asymptomatic to moderately symptomatic children after drowning. Eur J Pediatr. 2019;178(9):1379-1384.
- Wyckoff MH, Singletary EM, Soar J, et al; COVID-19 Working Group. 2021 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the Basic Life Support; Advanced Life Support; Neonatal Life Support; Education, Implementation, and Teams; First Aid Task Forces; and the COVID-19 Working Group. Resuscitation. 2021;169:229-311.
- Szpilman D, Bierens JJ, Handley AJ, Orlowski JP. Drowning. N Engl J Med. 2012;366(22):2102-2110.
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care – read the June issue of The Link.