Measles and Misinformation: A Double Threat to the New Year
Vaccine Update - January 2023
Column Author: Yvonne Carter, MSN, APRN, FNP-C | Infectious Diseases
Column Editor: Angela Myers, MD, MPH | Pediatric Infectious Diseases; Division Director, Infectious Diseases; Medical Director, Center for Wellbeing; Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
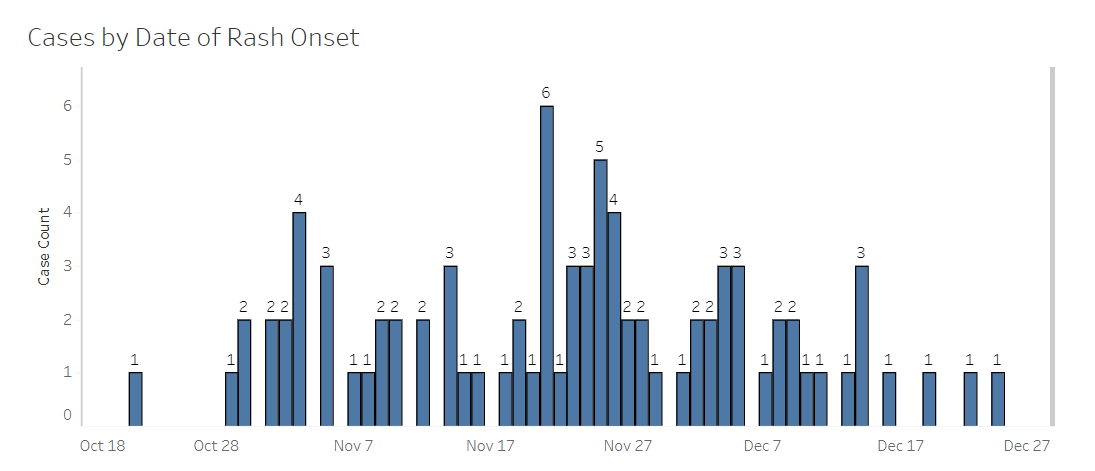
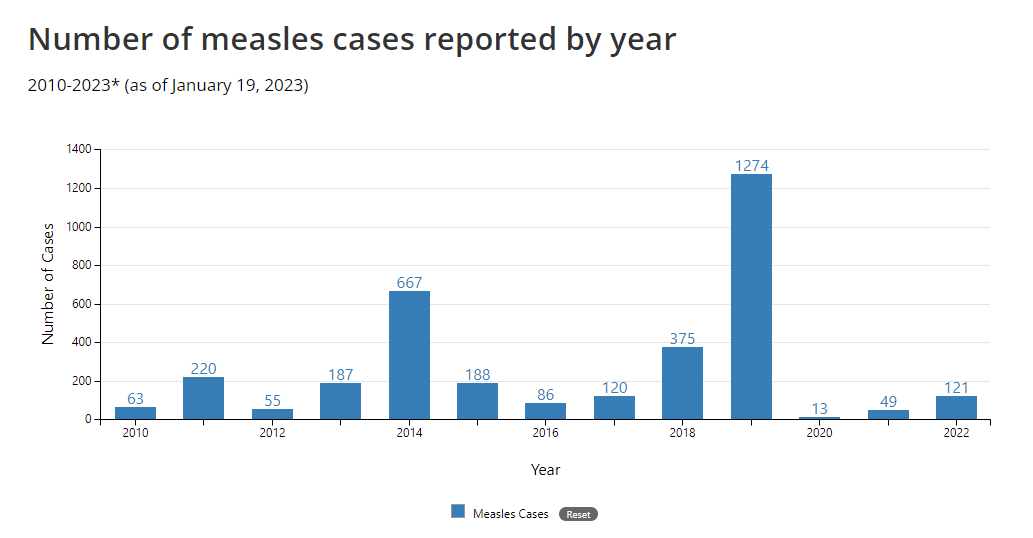
What is the New Year without a resolution? As we welcome 2023 and reflect on 2022, we celebrate great strides in the “wide world of vaccines” amid a continuous pandemic. Moving forward, we look to identify how we can improve. But we need look no further than central Ohio, where over 80 cases of measles have been reported since October — all in children under 18. (Figure 1) Ohio’s outbreak alone surpassed measles cases reported to the Centers for Disease Control and Prevention (CDC) in 2020 and 2021 combined (and accounts for nearly 70% of cases nationwide in 2022).1,2 (Figure 2)
Of the 82 cases reported as of the year’s end, 54 are in children ages 1-5, and 23 are in infants less than 12 months of age. Over 90% of cases (74 of 82) are in children entirely unvaccinated against measles. Of remaining cases, 5% are only partially vaccinated, and 5% are of unknown vaccination status. At the start of 2023, there have been no reported cases in a child fully vaccinated against measles.1
Figure 1. Ohio Outbreak Epidemiology Curve
The 23 infant cases in Ohio were not yet eligible for their first measles-mumps-rubella (MMR) vaccine dose, but what about the other 59 cases? Upon investigation, Columbus, Ohio, public health officials have found that while most cases are old enough for at least one dose of MMR vaccine, parents have chosen not to vaccinate their children.5 As discussed in the November 2022 issue of The Link, there has been an alarming drop in childhood vaccination rates since the start of the COVID-19 pandemic. Measles is no exception. In 2021, an estimated record high of 24.7 million children worldwide missed their first dose of measles-containing vaccine, with another 14.7 million missing their second.3 Officials are now calling measles an “imminent threat worldwide” due to the following:
- Declines in children receiving the measles vaccine
- Weakened surveillance
- Continued interruptions and delays in immunization activities due to COVID-19
- Persistent large outbreaks in 2022 — Ohio chief among them in the U.S.3
While the pandemic played its part, vaccine hesitancy — or strict refusal — was a threat to MMR vaccine coverage before COVID-19 emerged on the scene. First licensed in 1963, the same vaccine used today has been available since 1968, with over five decades of data proving safety and effectiveness.4 Yet in 2019 the U.S. nearly lost its measles elimination status for the first time since 2000, with 1,274 confirmed cases that year — the most since 1992.2,4 Columbus public health officials share that even before COVID-19, pockets of their community would opt against the MMR vaccine specifically, with vaccine refusal attributed to the ongoing misconception that it causes autism.5
Figure 2. U.S. Measles Cases 2010-2022
Anti-vaccine misinformation threatens the safety of children worldwide. Measles is highly contagious — one of the most contagious human viruses — and it is almost entirely preventable through vaccination. A minimum 95% vaccination rate is required for herd immunity to protect communities and maintain elimination of the disease. Globally, we are far from achieving this, with only 81% of children worldwide receiving their first dose of measles-containing vaccine, and only 71% receiving their second dose in 2021. This is the lowest worldwide measles vaccination coverage since 2008.3,5 Both doses of MMR vaccine are approximately 97% effective at preventing measles, and even just one dose protects at least 93% of children. Primary vaccine failure may occur in up to 7% of children after the first dose and is the reason why a second dose has been recommended before starting school. After two doses, a person is considered protected for life.6
The CDC considers those most at-risk for measles complications to include children under 5, adults over 20, pregnant women and people with compromised immune systems.7 Over 90% of children affected by the outbreak in Ohio fall into the most at-risk category. Because measles can stay in the air for up to two hours after an infected person was present, 90% of unvaccinated people exposed will become infected, and an estimated 1 in 5 of those will be hospitalized.6,7 Initial symptoms can appear within one to two weeks after contact with the virus and often include high fever, cough, runny nose, and red or watery eyes. A rash then appears three to five days after onset of initial symptoms.6 Of the 82 cases reported in Ohio, 32 have been hospitalized due to symptoms such as dehydration, diarrhea and pneumonia. Some have even spent the night in the intensive care unit.1,5 Other possible complications from measles include encephalitis and death, which have not yet been documented in any cases from Ohio.1,7 Due to the delay in symptom onset from time of exposure, it is likely we have not seen the last of this outbreak.
Until vaccine coverage improves in the U.S. and elsewhere, experts expect to see more measles outbreaks.5 The American Academy of Pediatrics (AAP) calls on health care providers to use direct and consistent communication with families to improve vaccine acceptance. We must emphasize to families that vaccines are safe and effective and explain how serious disease can occur in the unvaccinated.8 Our communications to both patients and communities must highlight the consequences of remaining unvaccinated against preventable diseases. Educating parents and families is the first step in improving vaccine acceptance, and there is no time more important than now. Let’s welcome 2023 by doing our part to protect all children from vaccine-preventable diseases.
References:
- Measles case summary: central Ohio outbreak. Ohio Disease Reporting System (ODRS). Accessed December 30, 2022. https://public.tableau.com/app/profile/columbus/viz/MeaslesPublicReport/MeaslesPublicReport
- Measles cases and outbreaks. Centers for Disease Control and Prevention. Accessed December 30, 2022. https://www.cdc.gov/measles/cases-outbreaks.html
- Nearly 40 million children are dangerously susceptible to growing measles threat. News release. Centers for Disease Control and Prevention; November 23, 2022. Accessed December 30, 2022. https://www.cdc.gov/media/releases/2022/p1123-measles-threat.html
- Measles history. Centers for Disease Control and Prevention. Accessed December 30, 2022. https://www.cdc.gov/measles/about/history.html
- Abbasi J. Amid Ohio measles outbreak, new global report warns of decreased vaccination during COVID-19 pandemic. JAMA. Published online December 15, 2022. doi:10.1001/jama.2022.23241
- Vaccine for measles. Centers for Disease Control and Prevention. Accessed December 30, 2022. https://www.cdc.gov/measles/vaccination.html
- Complications of measles. Centers for Disease Control and Prevention. Accessed December 30, 2022. https://www.cdc.gov/measles/symptoms/complications.html
- Edwards KM, Hackell JM; Committee on Infectious Diseases, the Committee on Practice and Ambulatory Medicine. Countering vaccine hesitancy. Pediatrics. 2016;138(3):e20162146. PMID: 27573088. doi:10.1542/peds.2016-2146
See all the articles in this month's Link Newsletter
Stay up to date on the latest developments and innovations in pediatric care -- read the January issue of The Link.
