A Real Headache
Outbreaks, Alerts and Hot Topics - January 2023
Column Author and Editor: Chris Day, MD | Pediatric Infectious Diseases; Director, Transplant Infectious Disease Services; Medical Director, Travel Medicine; Assistant Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
This past spring (May 2022), the Centers for Disease Control and Prevention (CDC) became aware that a number of clinicians around the country were concerned about a perceived increase in pediatric intracranial infections, including brain abscesses, epidural empyemas, and subdural empyemas caused by streptococci including, in particular, Streptococcus intermedius.1 Many such infections are associated with spread from a contiguous local source such as sinusitis or mastoiditis2 often preceded by respiratory viral infection. The CDC pursued two separate avenues of investigation, requesting reports of possible cases from health departments and from two provider listservs. The CDC also collaborated with the Children’s Hospital Association (CHA) to use the Pediatric Health Information System (PHIS, a database of inpatient encounters from CHA member hospitals) to examine trends in cases of intracranial infections from January 2016 to May 2022.
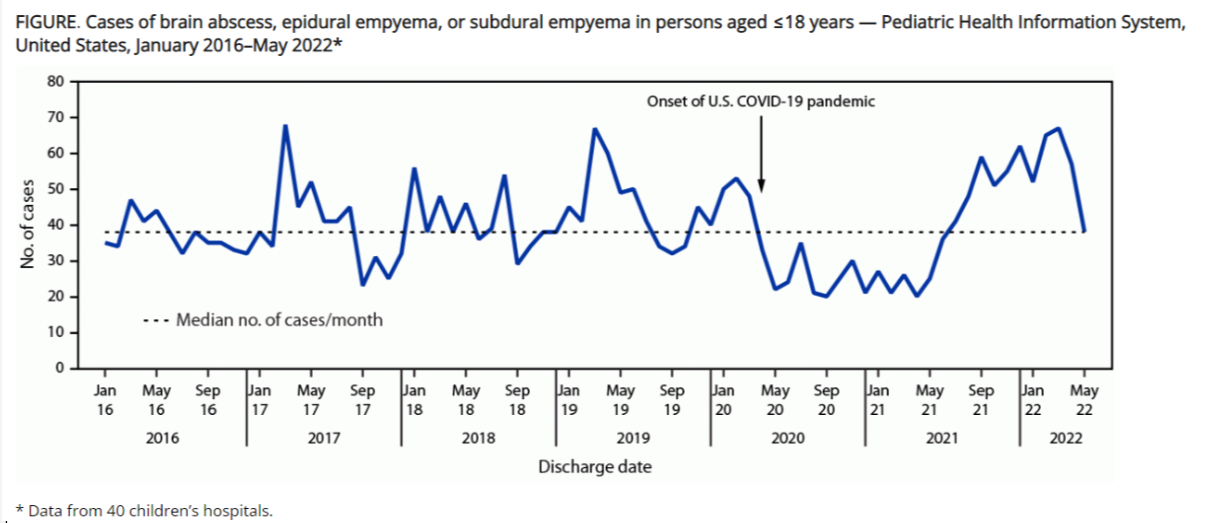
3,078 cases were identified from the PHIS database (Figure) with rates ranging from 20 to 68 cases per month (median = 38). From April 2020, monthly case counts were below the median for 15 months. Beginning in the summer of 2021, cases increased and remained above the median, peaking in March 2022. During the first period (April 2020 to July 2021), there were 184 fewer cases than would be expected based on the typical monthly median; in the second period (August 2021-May 2022) there were 177 more cases than would be typical. The March 2022 peak is similar in size to peaks seen in March of some prior years (2017 and 2019).
The CDC’s request resulted in the submission of 94 cases. Of those, 81 met CDC’s case definition of a brain abscess, epidural empyema or subdural empyema in a person aged ≤ 18 years without a previous neurosurgical procedure or history of head trauma. Available Streptococcus spp. specimens isolated from these cases were tested for antimicrobial susceptibility and underwent whole-genome sequencing. Streptococci were identified in most (92.1%) patients with positive cultures, commonly S. intermedius (41.6% of cases) and Streptococcus anginosus (18.4%). Nonstreptococcal species were also identified in 28.9% of these cases. Based on sequencing, the 15 S. intermedius isolates showed no apparent genetic relatedness. Nine of 16 S. intermedius isolates were pan-susceptible and only two were resistant to multiple antibiotics.1 These microbiologic findings are consistent with those seen typically in these infections.3
No overall increase in pediatric brain abscesses was noted over the period April 2020 to May 2022, but typical seasonal patterns were disrupted, likely related to changes in the circulation of viral respiratory pathogens during this part of the COVID-19 pandemic, first by nonpharmaceutical interventions designed to mitigate the pandemic and then by relaxation of those interventions. Concurrent COVID-19 was noted in between 1.3% and 10.9% of cases in the PHIS database (depending on the quarter examined), and COVID-19 was noted in the prior six weeks in 18.2% of the 81 cases reported to CDC.1
Pediatric brain abscesses, epidural empyemas and subdural empyemas are rare, serious infections always requiring hospitalization. They often occur as sequelae of less life-threatening infections of the paranasal sinuses or otic structures. Consequently, seasonal peaks of intracranial infections seem to follow peaks of respiratory viral illness.
These intracranial infections are frequently difficult to recognize clinically, especially early in their progression. It is common for the diagnosis to be delayed two weeks after the onset of symptoms, and delays can sometimes be much longer. Headache (present in 60%-70% of patients with brain abscess), fever (40%-60%), and focal neurologic deficits (35%-50%), the classic triad of brain abscess, are frequently not individually present and are found together in <30% of patients at the time of diagnosis. Vomiting is common (50%-60% of cases). Focal suppurative CNS infection should be considered when any three of the following are present: “fever, headache, nausea/emesis, increased ICP, altered consciousness, seizures (focal or generalized), or cranial nerve abnormalities.”3 Failure of complicated sinusitis or mastoiditis to respond as expected to therapy, especially if symptoms are rapidly progressive or if there is a change in neurologic status, may also suggest an intracranial focus. A head CT without contrast is not adequate to exclude the possibility of a brain abscess. Brain MRI is the preferred imaging modality when there is strong suspicion.3
References:
- Accorsi EK, Chochua S, Moline HL, et al. Pediatric brain abscesses, epidural empyemas, and subdural empyemas associated with Streptococcus species – United States, January 2016–August 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1169-1173. doi:10.15585/mmwr.mm7137a2
- Rivera K, Truckner R, Furiato A, Martinez S. The diagnostic challenge of the pediatric brain abscess. Cureus. 2021;13(6):e15402. doi:10.7759/cureus.15402
- Harrison CJ, Berkovich R. Focal suppurative infections of the nervous system. In: Long SS, Prober CG, Fischer M, Kimberlin DW, eds. Principles and Practice of Pediatric Infectious Diseases. 6th ed. Elsevier; 2022:337-347.
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care - read the January issue of The Link.