What if I have an Out-of-Network plan?
Thank you for choosing Children’s Mercy for your child’s health care needs. Your insurance has chosen not to include Children’s Mercy as an in-network provider. To get the most out of your insurance plan and to help lower your out-of-pocket costs, we recommend you follow the guide below.
To avoid higher out-of-pocket costs for your child's services, it is best to seek treatment with health care providers approved by your insurance plan or specific coverage network. To do this, call your health insurance plan and ask what providers are available in your coverage network. If your insurance says there are no providers in your network that can treat your child, follow the steps below.
Out-of-pocket cost comparison
Step 1: Request an out of network exception with your insurance plan
If your insurance company tells you there are no in-network providers that can treat your child or you would prefer that your child to be seen at Children’s Mercy regardless of providers available in your network, ask your insurance during your call how your child can receive an exception to be approved to seek care at an out of network provider and follow the steps that they outline for you.
*Please note: OON plans require patients to have an approved exception on file to receive care with an OON provider. This approval/exception must come from a provider who is in-network, such as a patient’s primary care provider (PCP). Children’s Mercy is unable to submit an OON exception. For the OON plan to start the exception process, your PCP will need to submit an OON referral or gap exception with your insurance plan. This is also true for out-of-state Medicaid plans.
*Please note: If you have a “Practitioner Only” plan or a plan that does not cover hospital-based or ancillary services, please see our Insurance page for additional information related to the pre-approvals.
*Please note: If the patient resides in a state other than Missouri or Kansas and has Medicaid insurance coverage through their state, please see our Insurance page for additional information related to the pre-approvals.
Step 2: Make notes of the insurance decision
If your out-of-network plan approves your request to be seen with an out-of-network provider, please ask for the approval or call reference number. Make note of the following information:
- Your exception request was: approved or denied
- If approved: exception approval number
- Call reference number
- Insurance rep’s name and phone number
Step 1: Fill out the CM Out-of-Network Appointment Request Form
Now that you have received a preliminary decision from your insurance plan, it’s time to request an approval with Children’s Mercy by filling out this form. Requesting appointment approval ensures the services your child needs will be prior-authorized and paid appropriately Obtaining a Single Case Agreement (SCA) allows your child to be scheduled. If your child’s insurance denied your request, this form is also used to provide you with a patient price estimate for services at Children’s Mercy without an approval from your plan.
Step 2: Children’s Mercy Financial Clearance team will process your request
Once you have completed and submitted the form, a member of the Children's Mercy Financial Clearance team will contact your insurance and request any prior authorizations that may be needed. Once the prior authorizations have been approved, we will initiate a Single Case Agreement (SCA) with your out-of-network plan. This process can take up to 30 days to complete.
Step 3: Financial Clearance will contact you to review insurance decision and to discuss next steps
If OON plan approves the terms of the Single Case Agreement request:
If your insurance approves for you to be seen at Children’s Mercy, you will be contacted by a member of the Financial Clearance team; you may proceed with scheduling appointment.
If OON plan does not approve the terms of the Single Case Agreement request:
If your insurance denies your request to be seen at Children’s Mercy, you may be able to continue as a self-pay (no insurance) patient. A Financial Clearance Specialist will walk you through this process after you fill out the Out of Network Request form mentioned in Step 3 above with the denial information, including providing you the estimated cost and payment requirements. Once you agree to the payment requirements, the Financial Clearance team member will transfer you to scheduling.
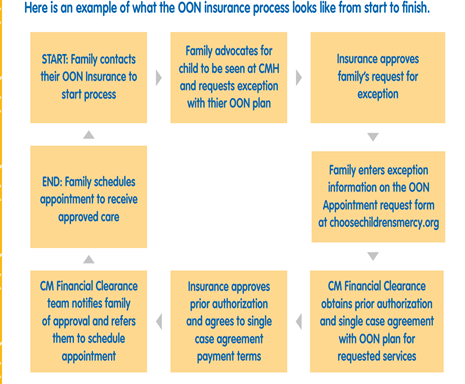
Here is an example of what the OON insurance process looks like from start to finish.
Prior-Authorization: Requirement for pre-approval from a payor to evaluate the medical necessity of services and/or determine benefit coverage prior to services. If a prior authorization is not obtained or approved, this could result in a reduction or denial of benefit coverage.
Referral: A pre-approval required from a Primary Care Provider (PCP) before seeking care from a specialist. If a referral is not obtained, and it is a requirement of the payor, this could result in a reduction or denial of benefit coverage.
Single Case Agreement (SCA): A reimbursement agreement between an uncontracted payor and Children’s Mercy for one instance, one appointment, and/or a specific timeframe for patient for care received at CM.
OON Exception: An approval by payor that services at Children’s Mercy are medically necessary for patient and will be paid at in-network benefit levels.
Out-of-State (OOS) Medicaid: Any Medicaid plan through a state outside of the states of Kansas or Missouri. Please refer to the full list of OON plans on our Insurance page to identify other states that may have special agreements with Children’s Mercy.
- Billing Process
- Contact Us
- Cost of Care Estimate Tool
- El Seguro
- FAQ: Understanding Health Care Costs
- Financial Assistance
- Financial Resources and Billing Information
- Guarantor Change Request Form
- Insurance Forms
- Insurance Plans and Coverage Types Accepted
- Insurance Terms and Definitions
- No Surprises Act
- Pay My Bill
- Questions to consider when selecting your health care plan
- Transition to Adulthood - Medical Insurance Choices for Adults
- Update Insurance Card or Demographics
- Your Visit
- Payment Types Accepted
