Anthrax
Outbreaks, Alerts and Hot Topics - January 2024
Column Author: Chris Day, MD | Pediatric Infectious Diseases; Director, Transplant Infectious Disease Services; Medical Director, Travel Medicine; Assistant Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
Column Editor: Angela Myers, MD, MPH | Pediatric Infectious Diseases; Division Director, Infectious Diseases; Medical Director, Center for Wellbeing; Professor of Pediatrics, University of Missouri-Kansas City School of Medicine; Clinical Assistant Professor of Pediatrics, University of Kansas School of Medicine
Anthrax is now extremely rare in humans in the United States, with only a single case confirmed from 2012-2018. However, anthrax continues to occur, sometimes in significant outbreaks, in other parts of the world, especially where vaccination of livestock against anthrax is less available or less practiced. In eastern Africa, there has been a recent outbreak in five countries (Kenya, Malawi, Uganda, Zambia and Zimbabwe) involving a reported nearly 1,200 human cases and 20 deaths. These victims are assumed to have been infected mostly by contaminated meat.
Bacillus anthracis, the causative organism of anthrax, is a gram-positive rod that forms resilient spores. It is most commonly an infection in domestic and wild ruminant mammals. When infected animals die from anthrax, the organism will be deposited in soil. In the spore form, anthrax can persist in the environment for decades. Animals contract anthrax by eating grass contaminated by spores. The current outbreak in eastern Africa has been attributed to heavy rainfall, an environmental condition that appears to contribute to transmission.1
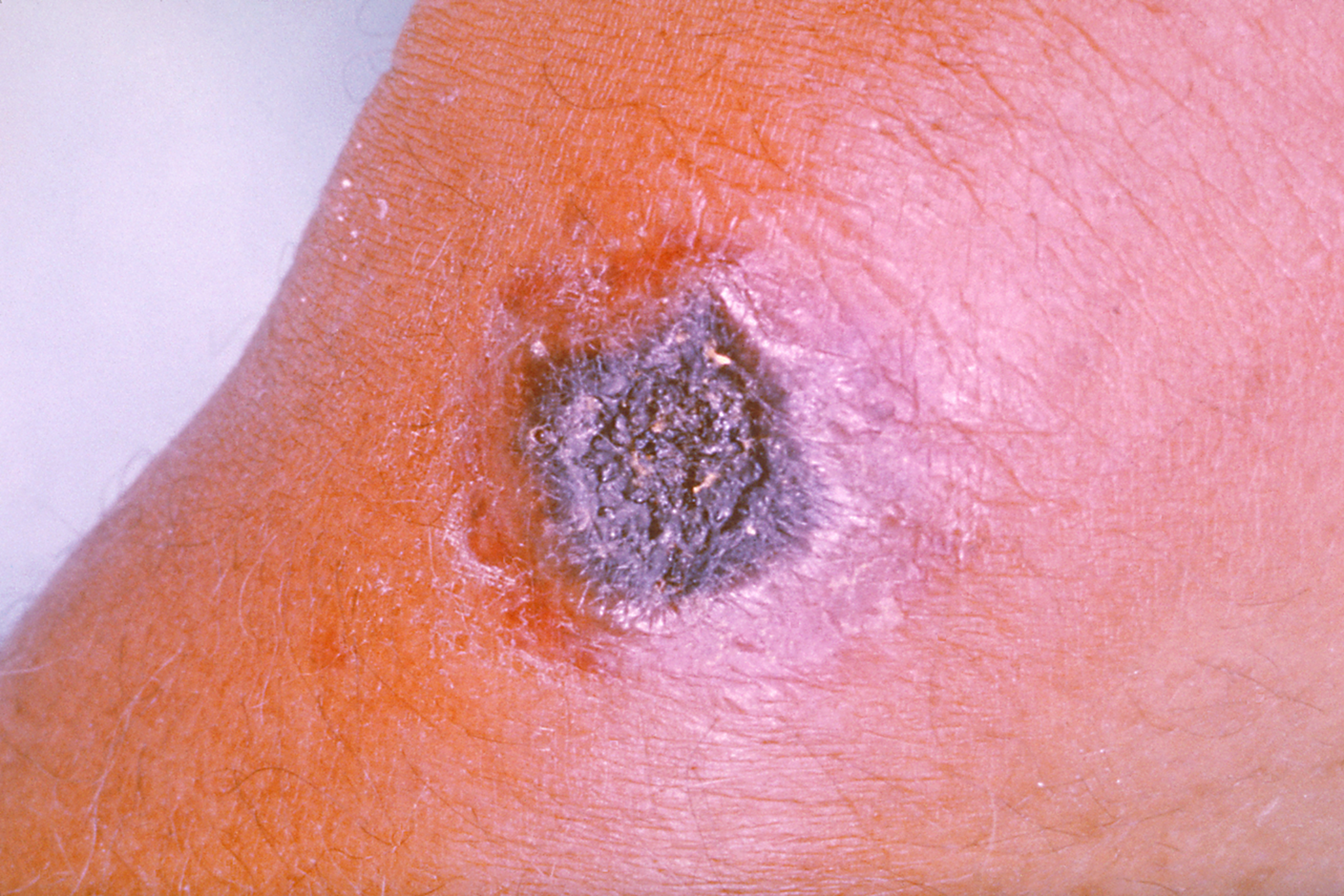
Naturally occurring transmission to humans occurs from contaminated animal products by skin contact, ingestion or inhalation. The route of transmission determines the early manifestations of illness. Cutaneous disease is the most common: anthrax is introduced either through breaks in the skin or perhaps through hair follicles. A small, painless, but frequently pruritic, papule forms and progresses to become vesicular or bullous. The lesion ultimately evolves into a necrotic ulcer (Figure 1) with a black eschar, often with impressive surrounding edema and regional adenopathy. Ingestion can lead to a gastrointestinal form of the disease that is similar to the cutaneous form except that the edema and ulceration occurs in gastrointestinal tract, usually the small bowel or colon. In the oropharyngeal form, necrotic ulcers covered with a pseudomembrane develop, often with pharyngeal and cervical swelling. Mortality with this form is significant. Aerosolization of anthrax can occur while working with wool or hides. Inhalation of small particles (<5 microns) can be deposited in the distal airways and alveoli and from there be transported to mediastinal lymph nodes by macrophages. Mediastinal infection often leads to bacteremia and, in as many as one-half of patients, to meningitis. Fulminant infection can lead to death within days. Any infection with anthrax has some potential to progress. In general, human-to-human transmission does not occur.
Not all infections with Bacillus anthracis have been unintentional. The most well-known use of anthrax as a weapon occurred shortly after the September 11, 2001, attacks on the World Trade Center and Pentagon. Letters containing infected powder were mailed to two U.S. senators and several media agencies, leading to 22 infections (11 cutaneous and 11 inhalational) and seven deaths (all of them inhalational cases). Anthrax remains a potential agent of bioterrorism.2
Partially in response to the 2001 anthrax attack, recommendations for treatment and post-exposure prophylaxis (PEP) have been revised. Recommended therapy prior to 2001 was often a single antibiotic, now recommended only for simple cases of cutaneous disease. Other forms of anthrax should be treated with a multidrug antibiotic regimen of at least two bactericidal antibiotics and an antibiotic that inhibits protein synthesis. Additionally, there are now three products available that neutralize anthrax toxins: anthrax immune globulin and two monoclonal agents, obiltoxaximab and raxibacumab. Use of these agents should be considered in consultation with the Centers for Disease Control and Prevention (CDC). Cutaneous disease of the head and neck is treated like systemic disease.3,4
In the event of an inhalational exposure, PEP includes the use of both multiple doses of an anthrax vaccine (BioThrax [Anthrax Vaccine Adsorbed (AVA)] is the only vaccine that it is currently anticipated would be used in children in the United States) and up to 60 days of antibiotic chemoprophylaxis (viable spores have been detected for up to 100 days in the lungs of primate animal models; disease has occurred as late as day 58).5
Anthrax is an immediately notifiable disease: clinicians must contact local or state health departments upon reasonable suspicion of the diagnosis. Health departments will assist with both diagnosis and treatment. Antitoxin therapy and vaccines are obtained with the assistance of health departments and the CDC.
Figure: Cutaneous anthrax (source: CDC PHIL/Dr. James H. Steele, in the public domain)
References:
- Mandavilli A. Mystery amid an anthrax outbreak in Africa. The New York Times. December 19, 2023. https://www.nytimes.com/2023/12/19/health/anthrax-africa.html
- History of anthrax. Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP). November 20, 2020. https://www.cdc.gov/anthrax/basics/anthrax-history.html
- Dixon TC, Meselson M, Guillemin J, Hanna PC. Anthrax. N Engl J Med. 1999;341(11):815-826. doi:10.1056/nejm199909093411107
- Committee on Infectious Diseases, American Academy of Pediatrics. Anthrax. In: Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH, eds. Red Book: 2021-2024 Report of the Committee on Infectious Diseases. 32nd ed. American Academy of Pediatrics; 2021:196-202.
- Bower WA, Schiffer J, Atmar RL, et al. Use of anthrax vaccine in the United States: recommendations of the Advisory Committee on Immunization Practices, 2019. MMWR Recomm Rep. 2019;68(4):1-14. doi:15585/mmwr.rr6804a1
See all the articles in this month's Link Newsletter
Stay up-to-date on the latest developments and innovations in pediatric care – read the January issue of The Link.