Minimally Invasive Pectus Excavatum Repair
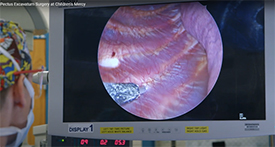
The Center for Pectus Excavatum and Carinatum in the Children’s Mercy Department of Surgery is one of the largest in the nation and performs the second highest number of corrective surgeries to repair pectus excavatum. All corrective surgeries are performed through a minimally invasive approach with a substernal bar (Nuss procedure) and cryoablation to enhance postoperative pain control. The Department of Surgery is involved in several multi-institutional studies, as well as department-sponsored clinical trials to improve both the technique and postoperative patient experience with minimally invasive repair of pectus excavatum (MIRPE).
Two randomized controlled trials have been completed at Children’s Mercy examining modalities for enhanced postoperative pain control comparing epidural pain control to patient-controlled analgesia (PCA). Results from these trials demonstrated adequate pain control within both groups and similar durations of hospital length of stay. These findings prompted modification of our technique for more efficient discharge and improved pain control with adoption of cryoablation, during which the intercostal nerves are frozen to cause a temporary paresthesia (numbness) that fully recovers post operatively. In a recent prospective trial, this technique demonstrated a significant decrease in hospital length of stay as compared to epidural and PCA modalities (1 day vs. 4.3 days vs. 4.2 days, respectively), and time to oral pain medication.
The Department of Surgery has multiple, ongoing studies to follow patients who undergo MIRPE with cryoablation to better understand the development, progression and variation of postoperative symptoms to identify how we may better provide anticipatory guidance for their postoperative course. With this data we can identify and possibly mitigate development of common symptoms that are found to impact daily activities to a greater extent than previously thought. This has the potential to decrease postoperative phone calls and emergency department visits, as well as provide a more comfortable postoperative experience for patients who undergo pectus excavatum repair.
Read the publication on postoperative pain control modalities for pectus excavatum repair.
