Wide World of Vaccines
June 2022
SARS-CoV-2 Vaccine and Final Musings as We Enter the Endemic Part of the Pandemic

Column Editor: Christopher Harrison, MD | Professor of Pediatrics, UMKC School of Medicine | Clinical Professor of Pediatrics, University of Kansas School of Medicine
This is my last column for Wide World of Vaccines, so bear with me if I seem a bit nostalgic.
The country has moved on to acceptance of COVID-19 as an ongoing part of life. People who have been oh-so-careful to not get COVID-19 are getting it despite still being careful. These infections are occurring because most cases now are spread from asymptomatic or minimally symptomatic (“I thought it was my allergies”) persons. Stadiums are full, throngs of people are at amusement parks and at sporting events, and requirements for vaccines and testing are melting away, even for international travel.
The “normalization” of SARS-CoV-2, it seems, is close to a done-deal. And that isn’t all bad. Two years is a long time to deal with the stress of radically altered ways of living. In fact, the pandemic is down to fifth place on many people’s worry list, making way for inflation, gas prices, supply chain issues and Putin’s war on Ukraine. But there are still a couple of downers along with compensating bright spots to keep in mind with the pandemic as we experience the rebirth of more normal activities going into summer 2022.
Downer 1: Ongoing evolution of Omicron variants. As we discussed in the last column, Omicron now has three subvariants circulating in the U.S. (B.2.12.2 currently dominating the Midwest, and BA.4 and BA.5 quickly rising on the coasts and emerging in the Midwest). Omicron has undergone what some call an evolutionary “sprint” so that BA.4 and BA.5 are so different from prior variants, including their immediate predecessor BA.2, that “natural immunity” from prior infections is nearly nonexistent. One headline referred to the need to “start from scratch” if a person’s only immunity is from prior infections.
Bright spot 1: Vaccines still work. In the face of disappointment over “natural immunity” from infection alone comes the realization that three doses of an mRNA vaccine nearly eliminate the chance of death-by-COVID-19 in otherwise healthy people regardless of the variant, for what appears to be a year after the last dose. Four doses seem to come close to the same result for those at higher risk (elderly, those with underlying conditions, and modestly immune-compromised persons). Further, the chance of hospitalization in otherwise healthy folks with three doses appears to be less than 10%, but hovers around 25% for high-risk groups.
Another related vaccine bright spot is that hybrid immunity (previously infected persons getting two or more doses of mRNA vaccine) is at least as good as three or four doses of mRNA vaccine – and likely a bit better than vaccine alone. So, getting infected after having been vaccinated could be considered like another booster – as long as one doesn’t get too sick or suffer long-COVID.
Downer 2: Omicron’s new variants are more contagious. The COVID-19 case rates are rising again after a lull post-January 2022’s BA.2 surge. How high they will go is yet to be determined, especially since BA.1.12.2 is more contagious than BA.2, and BA.4/BA.5 are more contagious than BA.2. So being indoors in the same room with an infected person renders two to three times the chance for acquiring the virus compared to, for example, the old Delta variant. And minimally or asymptomatic infected persons have high enough viral loads to spread almost as efficiently as symptomatic infected persons. The new Omicron variants also appear to replicate longer in unvaccinated than vaccinated persons, i.e., approximately 10 days in unvaccinated but approximately six days in vaccinated, regardless of symptoms.1
Bright spot 2: New Omicrons are not as virulent as Omicron BA.2 or Delta. We are seeing a notable but as yet modest rise in hospitalizations, even in children, nationally and also in the Midwest (Centers for Disease Control and Prevention Region 7 that includes Kansas and Missouri). Figure 1a. But deaths are not rising commensurate with rises in cases or hospitalizations. Figure 1b. This is likely due in part to Omicron’s proclivity for replication mostly in the upper not lower airways, so severe pneumonia and multiorgan failures are much less frequent and occur mainly in high-risk persons. Not surprisingly, though, Omicron has also been more likely to cause croup in young children than do other variants due to its upper airway focus. But multisystem inflammatory syndrome in children also appears to be less frequent, particularly in vaccinated children,2 and changes in smell and taste are also less frequent in all ages.3
The other reason for fewer deaths is that treatment works. We have come a long way since late 2021. The judicious outpatient use of monoclonal antibody (Evusheld is the only one currently showing effectiveness) and antivirals (e.g., Paxlovid taken within five days of symptom onset is ~75% effective in reducing hospitalization and death and reduces shedding during use) is making a difference, although their use is not as widespread as they should be. Test-to-treat sites and increased availability of antivirals should continue to reduce severe disease/death rates going forward. Likewise, steroids, and biologic anti-inflammatories along with better management of respiratory support are also key elements in reducing mortality and shortening hospitalizations.
My takeaway in this new less frantic era of the pandemic:
- SARS-CoV-2 is here to stay in some form and will produce modest surges regardless of time of year due to newly emerging variants; it won’t be a “simple” seasonal virus like influenza.
- Mild and asymptomatic infections are even more common now than last year and are still efficiently transmitting virus, so avoiding symptomatic folks will reduce risk of acquisition but is a less sure thing.
- Newly selected variants evade existing immunity in regional populations where infections are frequent, whether the existing immunity is from prior infection or vaccine. The selected virus is more likely to evade immunity from infection alone, as opposed to vaccine or vaccine plus prior infection. We need to try to reduce chances of a new variant by continuing to try to reduce case rates. We also need to keep pushing vaccine worldwide – and now, particularly for our younger pediatric patients, as emergency use authorizations are now in place for children 6 months of age and older.
- We need to develop our own standard operating procedures in our practices/clinics/institutions to promote vaccines and outpatient treatment. Individually, we need to be comfortable answering questions from families – even questions about adults because they can be vectors for children.
- High-risk and unvaccinated persons remain a cause for concern. High-quality masks will remain a recommendation for the foreseeable future for these persons, particularly when indoors with persons who may be infected. Social tolerance for those who feel the need to wear masks is important.
Now, as I complete my last column, I have some wishes to send to you. I wish for you to enjoy your summer with loved ones as much as you can. I wish that you try not to dwell on the negatives of politics or the economy. I wish that you follow a tenet of mine: Do something every day that not only is fun but is also a source of true joy. Happy summer.
Figure 1a. Hospitalization rate in children from Region 7, mid-2021-June 9, 2022.4
Data source: CDC COVID Data Tracker: New Hospital Admissions (accessed June 13, 2022)
Figure 1b. Death rate from SARS-CoV-2 disease in Missouri, Jan. 2020-June 20, 2022.4
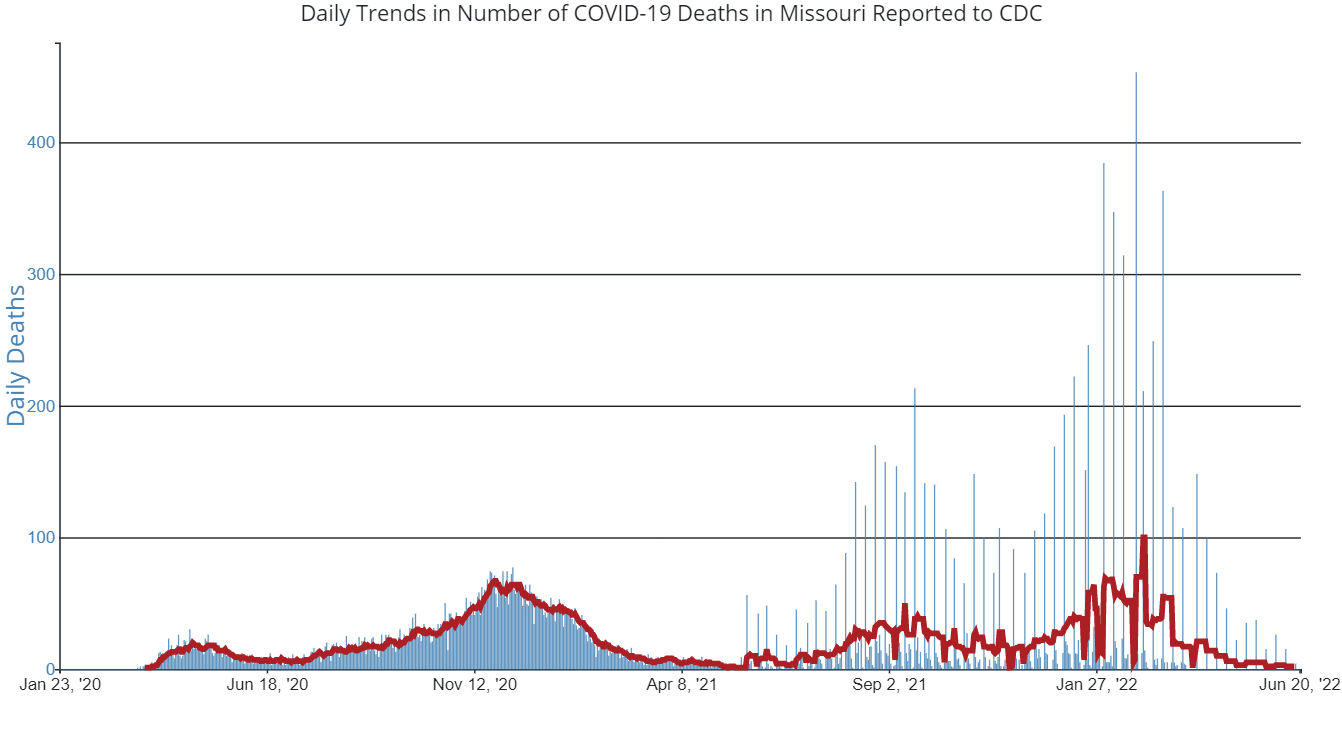
Blue vertical lines are daily deaths. Red horizontal line is daily death trend.
Data source: CDC COVID Data Tracker: Daily Deaths (accessed June 21, 2022)
References:
- Takahashi K, Ishikane M, Ujiie M, et al. Duration of infectious virus shedding by SARS-CoV-2 Omicron variant-infected vaccinees. Emerg Infect Dis. 2022;28(5):998-1001. doi:10.3201/eid2805.220197
- Holm M, Espenhain L, Glenthøj J, et al. Risk and phenotype of multisystem inflammatory syndrome in vaccinated and unvaccinated Danish children before and during the Omicron wave. JAMA Pediatr. Published online June 8, 2022.
- Coelho DH, Reiter ER, French E, Costanzo RM. Decreasing incidence of chemosensory changes by COVID-19 variant. Otolaryngol Head Neck Surg. Published online May 3, 2022.
- Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: US Department of Health and Human Services, CDC; 2022, June 13. https://covid.cdc.gov/covid-data-tracker