What's the Diagnosis?
November 2022
Visual Diagnosis

Column Author: Angela Myers, MD, MPH | Director, Division of Infectious Diseases | Professor of Pediatrics, UMKC School of Medicine | Medical Editor, The Link Newsletter
Column Editor: Joe Julian, MD, MPHTM, FAAP | Hospitalist, Internal Medicine – Pediatrics | Clinical Associate Professor, Internal Medicine and Pediatrics, UMKC School of Medicine
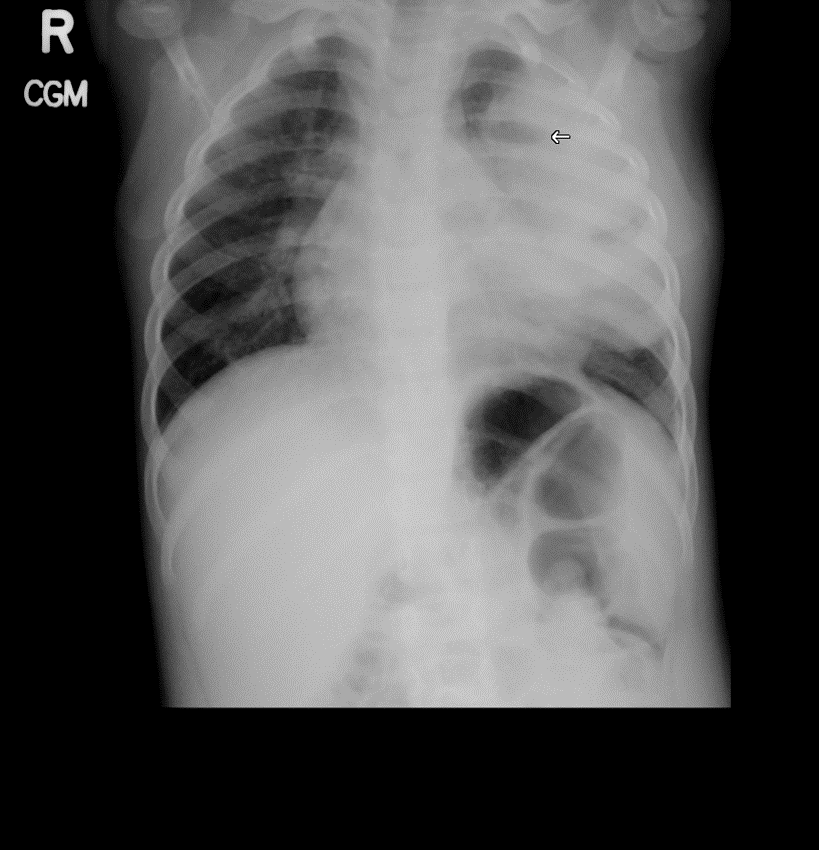
A 2-year-old female presents with a one-week history of fever up to 39.3 C, cough, malaise and decreased oral intake. She is fussy and tired on exam, but not toxic appearing. The family denies history of choking, but she has had emesis twice in the last two days. She has fever of 38.7 C with mild tachycardia and tachypnea. Lung exam is significant for diminished breath sounds in the left upper lobe with some crackles noted. She is fully immunized, including influenza vaccine. Chest radiograph obtained in the office is shown below.

Of the following, the most likely diagnosis for this patient is:
- Necrotizing pneumonia with lung abscess
- Pneumonia with empyema
- Reaction to an inhaled foreign body
- Uncomplicated left upper lobe pneumonia
The correct answer is: A. Necrotizing pneumonia with lung abscess
The patient in the above vignette has a left upper lobe pneumonia which evolved into a lung abscess. The initial CXR revealed a small air/fluid level (denoted by arrow), and the chest computed tomography provided a more detailed view of the abscess. The lung bases on both sides are clear, indicating that effusion and/or empyema is not present. While this child could have a foreign body in the lung, her clinical presentation is more consistent with acute pulmonary infection, rather than low-grade fever and more indolent findings that may be seen with the setting of aspiration.
Uncomplicated pneumonia versus lung abscess is an important distinction when determining length of treatment for pneumonia, as uncomplicated lobar pneumonia may be treated with shorter courses (5 days) of antibiotics, compared to the need for longer term therapy (two to four weeks) in the setting of lung abscess.1,2 When present, empyema is often drained for both diagnostic and therapeutic purposes. However, lung abscess with necrotizing pneumonia is typically treated medically, as there is concern for development of bronchopulmonary fistula with ongoing air leak. Additionally, most lung abscesses will drain naturally through the bronchial tree and heal without surgical intervention. Drainage should be considered for large abscesses (>6 cm) or those that do not resolve with optimized antibiotic therapy. Surgical resection may be needed in the setting of secondary lung abscess.3
The causes of lung abscess can be defined as primary and secondary in children. The majority of lung abscesses in children are primary, resulting from bacterial pneumonia, as in the case above. Secondary lung abscess results from underlying structural lung abnormalities (e.g., congenital cystic malformations). There is significant overlap of bacterial etiologies between primary and secondary lung abscess. While primary lung abscess may be caused by a single pathogen, such as Staphylococcus aureus, Streptococcus pyogenes or Streptococcus pneumoniae (although rare), anaerobic bacteria may also be found.4 In contrast, nearly all secondary lung abscesses are polymicrobial in nature, with oral flora playing a main role. Combination penicillin with a beta-lactamase inhibitor (e.g., ampicillin-sulbactam) generally provides adequate empiric antimicrobial coverage. An agent that provides methicillin-resistant S. aureus (MRSA) coverage should be considered when clinical suspicion of MRSA is high.
References:
- Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-e76.
- Williams DJ, Creech CB, Walter EB, et al. Short vs. Standard-Course Outpatient Antibiotic Therapy for Community Acquired Pneumonia in Children: The SCOUT CAP Randomized Clinical Trial. JAMA Peds. 2022;176(3):253-261.
- Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. 2015;3(13):183.
- Choi MS, Chun JH, Lee KS, Rha YH, Choi SH. Clinical characteristics of lung abscess in children: 15-year experience at two university hospitals. Korean J Pediatr. 2015;58(12):478-483.
