What's the Diagnosis?
May 2021
Visual Diagnosis

Author: Kristin Streiler, MD
Column Editor: Joe Julian, MD, MPHTM, FAAP | Hospitalist, Internal Medicine - Pediatrics | Assistant Professor, Internal Medicine and Pediatrics, UMKC School of Medicine
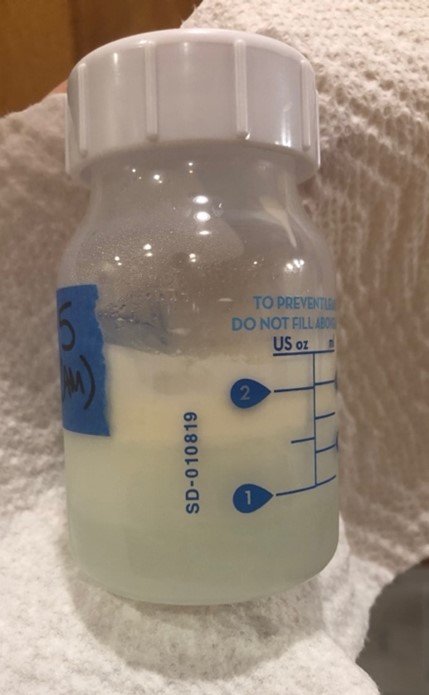
During a 6-month well-child check for a healthy baby girl, her mother produces the bottle of expressed breast milk pictured below. Her mother reports she received the first dose of the Pfizer/BioNTech COVID-19 vaccine two days ago. She expressed the milk pictured below yesterday and stored it in her refrigerator overnight. This morning, she noticed the milk appears blue and is worried it has been affected by her recent vaccination. She asks your advice about whether to feed her baby the milk and whether she can proceed with the second dose of the vaccine in a few weeks.
Which of the following is the most appropriate response?
A. The milk is contaminated by the vaccine. It should be discarded rather than fed to the baby. If she wishes to continue breastfeeding, she should refrain from receiving the COVID-19 vaccine.
B. The blue appearance of the milk is normal for human milk and unrelated to the vaccine. It may be fed to the baby as usual. Numerous medical and public health societies have advised that lactating people can receive a COVID-19 vaccine.
C. The blue appearance of the milk is abnormal. It should be discarded rather than fed to the baby. If she chooses to proceed with the second dose of the vaccine, then she should “pump and dump” for 24 hours following vaccination.
D. The blue appearance of the milk is normal for human milk. It may be fed to the baby as usual. Lactating mothers must wait for full FDA approval of the vaccine before receiving it.
Answer: B. Mature breast milk is typically bluish-white and may separate during storage in a refrigerator. There is a wide range of normal for color of breast milk, and changes in color may be related to the mother’s diet and/or the presence of blood, most commonly due to nipple trauma.1
Even though the clinical trials for COVID-19 vaccines currently authorized under an EUA in the United States did not include people who are breastfeeding, there is no biologically plausible mechanism for how these vaccines would pose a risk to lactating people or their children. Thus, the Centers for Disease Control (CDC),2 American Academy of Pediatrics (AAP),3 American College of Obstetricians and Gynecologists (ACOG),4 Academy of Breastfeeding Medicine (ABM),5 and World Health Organization (WHO)6 recommend lactating people who meet criteria for vaccination be offered a COVID-19 vaccination because “theoretical concerns regarding the safety of vaccinating lactating individuals do not outweigh the potential benefit of receiving the vaccine.”5
Furthermore, two recent studies7,8 have demonstrated robust vaccine response in lactating people. Both studies confirmed the presence of vaccine-generated antibodies to SARS-CoV-2 in breast milk, which may confer an immune benefit to breastfeeding infants and children. Vaccine-generated antibody titers were higher than those induced by SARS-CoV-2 infection.7
According to the ABM, there is no biologically plausible mechanism for a COVID-19 vaccine to contaminate breast milk. Additionally, disruption of breastfeeding may harm the dyad. There is no reason to pause breastfeeding or “pump and dump” milk for any period of time following vaccination.5
References:
- Australian breastfeeding association. Unusual appearances of breast milk. 2017. https://www.breastfeeding.asn.au/bfinfo/unusual-appearances-breastmilk.
- CDC. Information about COVID-19 vaccines for people who are pregnant or breastfeeding. Updated 28 April 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html.
- AAP. American Academy of Pediatrics Guidance: The COVID-19 vaccine is safe, effective and should be given to all who are eligible. 2 February 2021. https://services.aap.org/en/news-room/news-releases/aap/2021/american-academy-of-pediatrics-guidance-the-covid-19-vaccine-is-safe-effective-and-should-be-given-to-all-who-are-eligible/.
- ACOG. Practice advisory: Vaccinating pregnant and lactating patients against COVID-19. Updated 28 April 2021. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/vaccinating-pregnant-and-lactating-patients-against-covid-19.
- ABM. Statement: Considerations for COVID-19 vaccination in lactation. 14 December 2020. https://abm.memberclicks.net/abm-statement-considerations-for-covid-19-vaccination-in-lactation.
- WHO. Pfizer BioNTech COVID-19 vaccine: what you need to know. 20 April 2021. https://www.who.int/news-room/feature-stories/detail/who-can-take-the-pfizer-biontech-covid-19--vaccine.
- Gray et al. COVID-19 vaccine response in pregnant and lactating women: a cohort study. American Journal of Obstetrics and Gynecology (2021), doi: https:// doi.org/10.1016/j.ajog.2021.03.023.
- Perl et al. SARS-CoV-2-specific antibodies in breast milk after COVID-19 vaccination of breastfeeding women. JAMA. Published online April 12, 2021. doi: 10.1001/jama.2021.5782.
