Outbreaks, Alerts and Hot Topics
May 2022
The Rising Tide of Sexually Transmitted Infections During the COVID-19 Pandemic
Column Editor: Angela Myers, MD, MPH | Director, Division of Infectious Diseases | Professor of Pediatrics, UMKC School of Medicine | Medical Editor, The Link Newsletter
Surveillance for sexually transmitted infections (STIs) decreased in 2020 due to reduced screening capabilities and to the shift of public health resources to COVID-19 testing and tracking. These changes led to underreporting for chlamydia, gonorrhea and syphilis in early 2020, with a rebound for both gonorrhea and syphilis later in the year as health care clinics reopened.1 Interestingly, chlamydia diagnoses did not rise in late 2020 like gonorrhea and syphilis diagnoses did (Figures 1-3),2 which may be related to the fact that chlamydia infections are more likely to be asymptomatic. So, when STI screening dropped in the early pandemic, there were fewer opportunities to identify chlamydia than gonorrhea and syphilis, since people with symptoms (more likely in the latter two) were more likely to seek out testing and treatment. Additionally, testing for gonorrhea and syphilis was prioritized over chlamydia testing by many health departments as they tried to balance the need for ongoing COVID-19 work in the face of staffing shortages. Therefore, it isn’t surprising that reported chlamydia cases were down 13% overall and that reported cases of gonorrhea and syphilis were up 10% and 7% respectively. (Figures 1-3)
The increase in syphilis cases was even more pronounced in women of childbearing age, with a 24% increase (5,726 cases in all stages) from 2019 to 2020, which then led to a 15% increase in congenital syphilis cases (2,148 cases) with 150 congenital syphilis-related deaths. The preliminary data for 2021 does not look better. Based on early reporting to the Centers for Disease Control and Prevention (CDC) (data will not be finalized until fall 2022), 33 states have reported an increase in syphilis cases, with 2,268 cases of congenital syphilis and 166 deaths from congenital syphilis.3 (Figures 4-5)
Recently, the U.S. Preventive Services Task Force (USPSTF) updated its guidelines for chlamydia and gonorrhea screening to include sexually active women and men 24 years and younger, as well as adults 25 years and older who have an increased risk of infection (e.g., new partner, more than one partner, inconsistent condom use).4
Because chlamydia infections are most common in women 15-24 years of age, screening should be performed for this population at any visit in which new or persistent risk factors have surfaced since the last negative test result.4 Thus, a teenager may need to be tested after the onset of sexual activity and again with any new partner and again if they develop symptoms.
USPSTF screening recommendations for syphilis are currently being updated from the previous 2016 version. The 2016 guidelines recommend screening for syphilis in nonpregnant women and adolescents with an identified risk factor (e.g., incarceration, commercial sex work), males <29 years of age, transgender or gender diverse people, those who live in certain geographic areas (Southern states have the largest proportion and Western states have the highest rate), and those who belong to certain racial/ethnic groups (e.g., Black, Hispanic, American Indian/Alaska Native).4,5
All pregnant women should be screened for STIs. A recent study characterizing pregnant women with syphilis found that presence of psychiatric illness and history of non-injection drug use (primarily marijuana) were associated with a five-fold increase in congenital syphilis.6 Late prenatal care (first visit in second trimester) was also associated with a two-fold increase in congenital syphilis, as well as treatment later in the pregnancy. These findings may be related, in part, to barriers to access to care for women with psychiatric illness. Interestingly, having a history of syphilis was associated with lower odds of congenital syphilis (0.1, 95% CI 0.02-0.50), which may be related to increased patient and provider awareness and thus enhanced screening in people who have a history of syphilis.
How well are we doing as pediatricians in screening sexually active adolescents for STIs? Not great. A group of researchers in Chicago analyzed the results of the 2019 National Youth Risk Behavior Survey, which asked about STI testing, excluding human immunodeficiency virus (HIV) testing, in the previous 12 months among 2,500 sexually active adolescents. Overall, only 20% of sexually active teenagers had STI screening in the previous year (26% females vs. 13.7% males).7 While testing did increase with age from 12.6% in ≤15 years to 37% in ≥18 years, and some risk factors seemed associated with increased likelihood of testing (e.g., same-sex male sexual contacts, higher number of recent or lifetime partners), screening is still far below what is recommended for these groups.7 These survey data are pre-COVID-19 pandemic and based on CDC data; it is reasonable to suspect that screening may have been even lower during the pandemic, though we have no current data.
Routine screening of sexually active adolescents is an important part of preventive health care visits aimed at identifying early (even asymptomatic) infections to prevent development of symptoms or pelvic inflammatory disease, to reduce transmission to partners, and to prevent congenital and neonatal infections. Routine chlamydia testing of sexually active 16- to 24-year-olds is a Healthcare Effectiveness Data and Information Set (HEDIS) measure that offices/clinics can use to prompt clinicians to obtain testing. We can hope that such prompts would also trigger testing for other STIs, including gonorrhea, syphilis and HIV. If your practice does not currently have a standardized approach to STI screening of adolescents, now is a good time to consider how best to implement routine STI testing into your practice.
Figure 1. Cases of chlamydia reported in 2020 as a percentage of 2019 by MMWR week
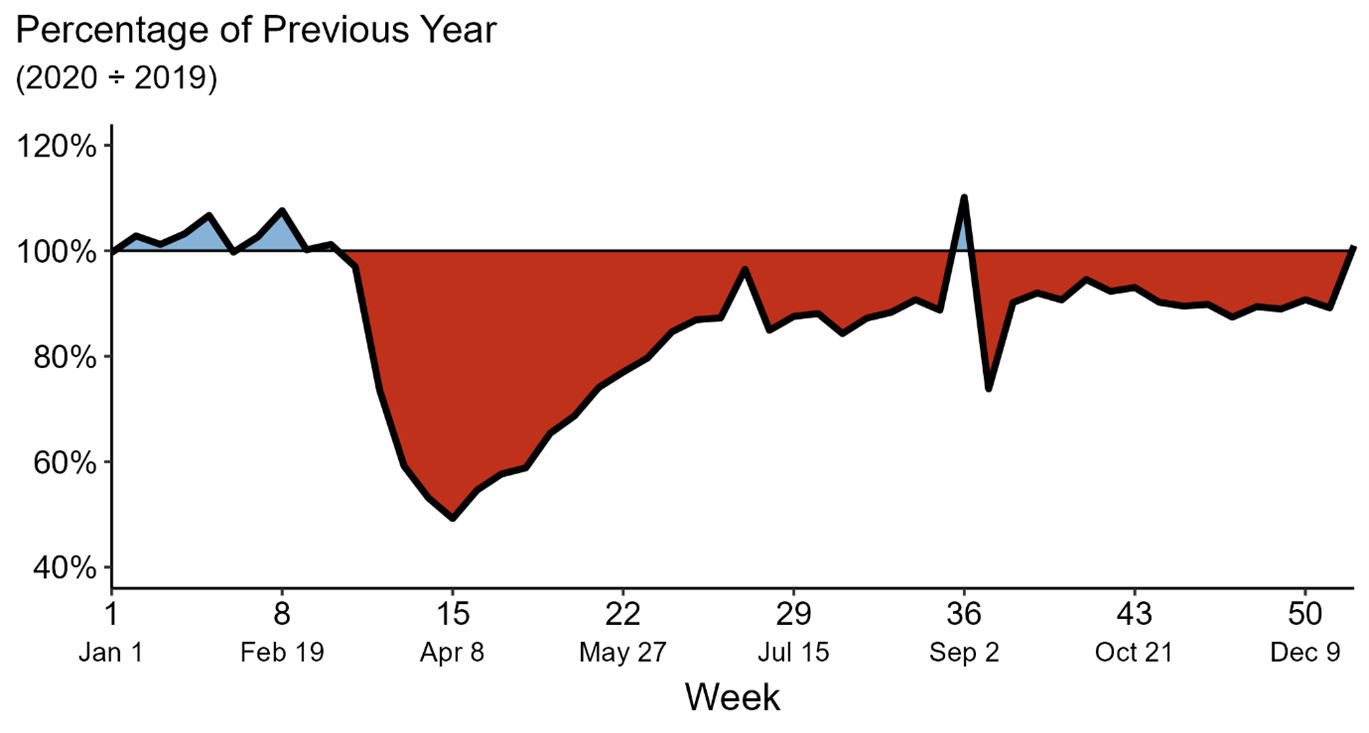
Source: Reference 2 (CDC: Impact of COVID-19 on STDs)
Figure 2. Cases of gonorrhea reported in 2020 as a percentage of 2019 by MMWR week
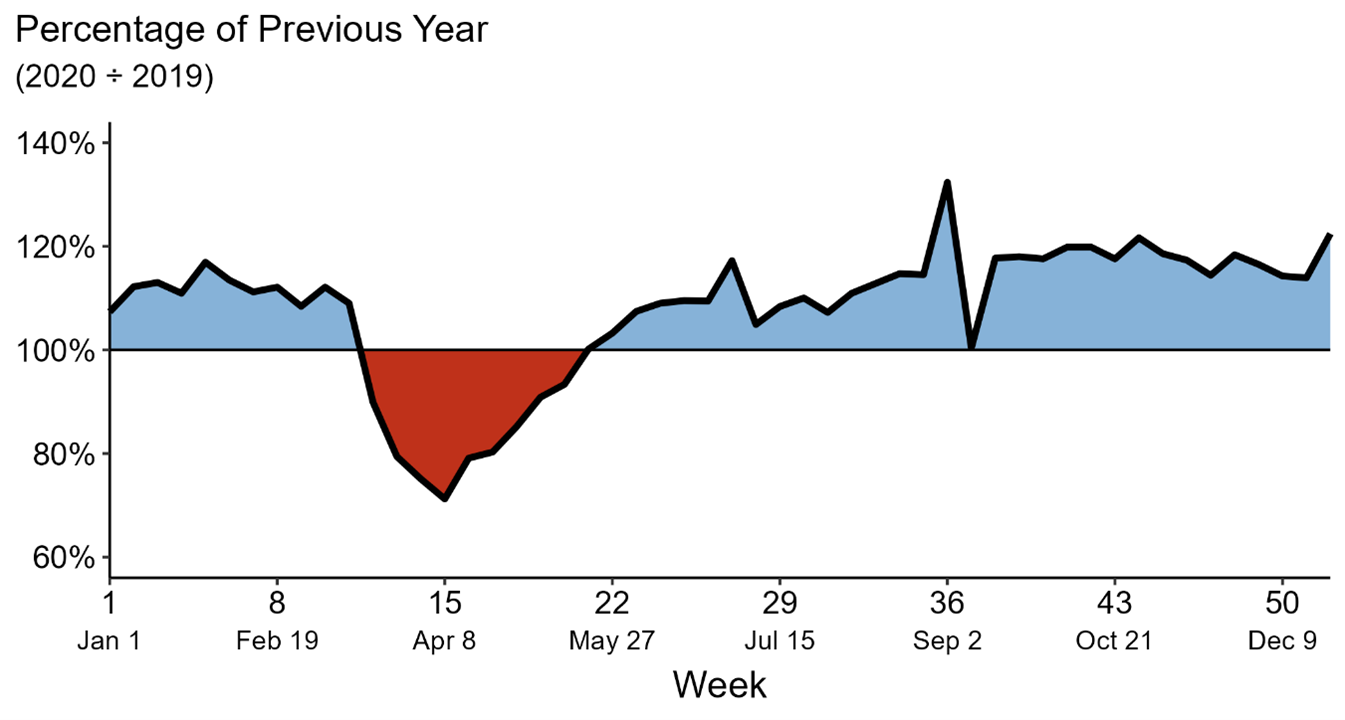
Source: Reference 2 (CDC: Impact of COVID-19 on STDs)
Figure 3. Cases of syphilis reported in 2020 as a percentage of 2019 by MMWR week
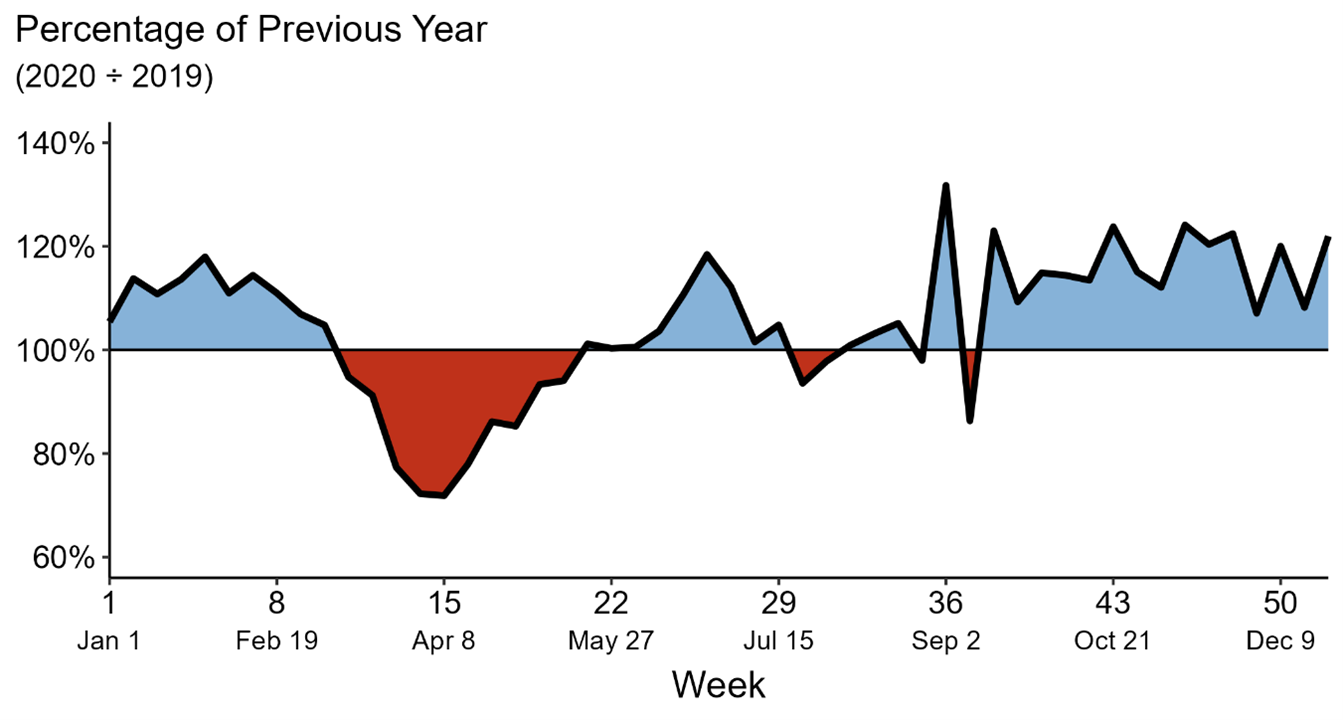
Source: Reference 2 (CDC: Impact of COVID-19 on STDs)
Figure 4. Congenital syphilis cases reported by birth year, United States, 2011-2021
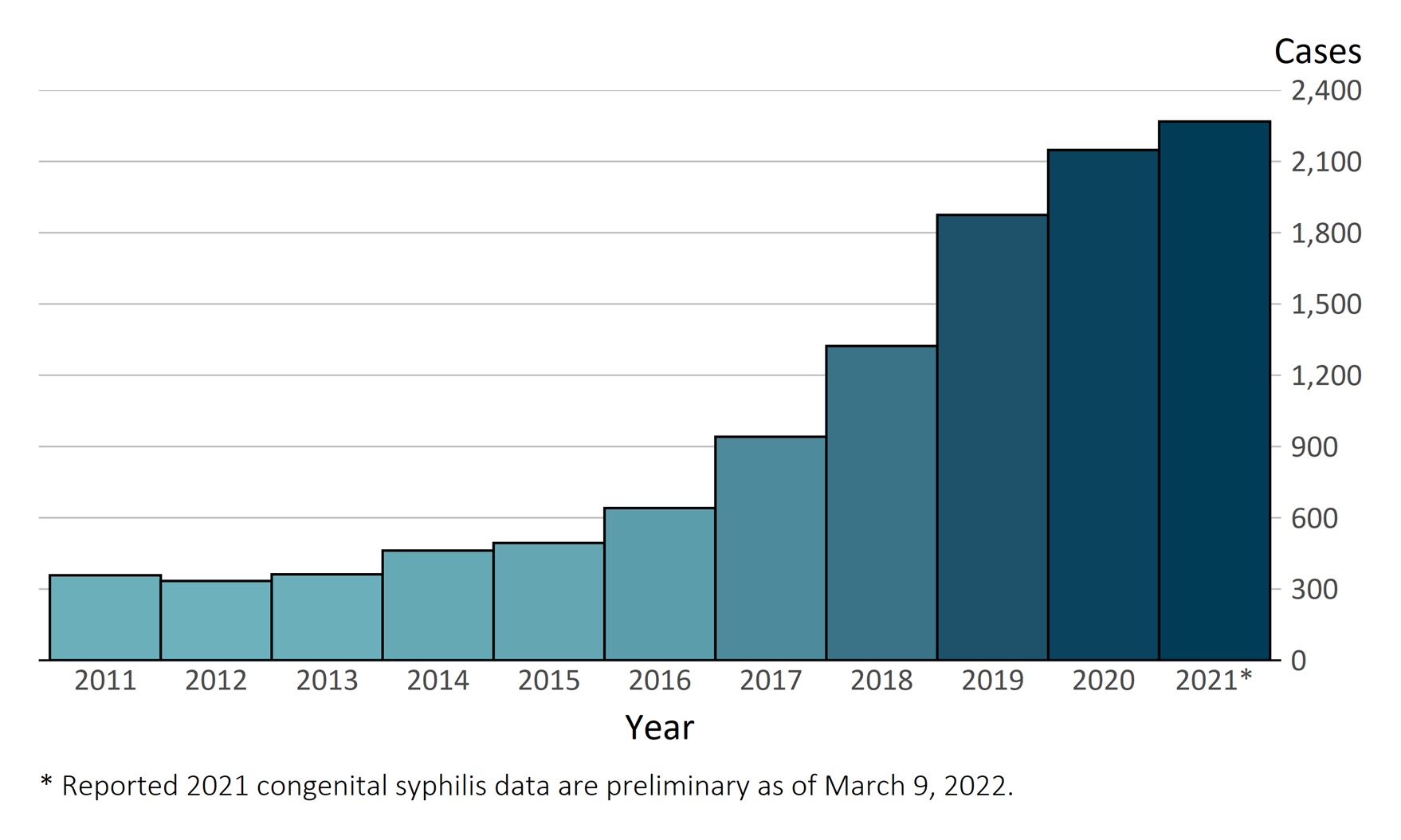
Source: Reference 3 (CDC: Preliminary 2021 Data: Syphilis)
Figure 5. Congenital syphilis stillbirths and infant deaths reported by birth year, United States, 2011-2021
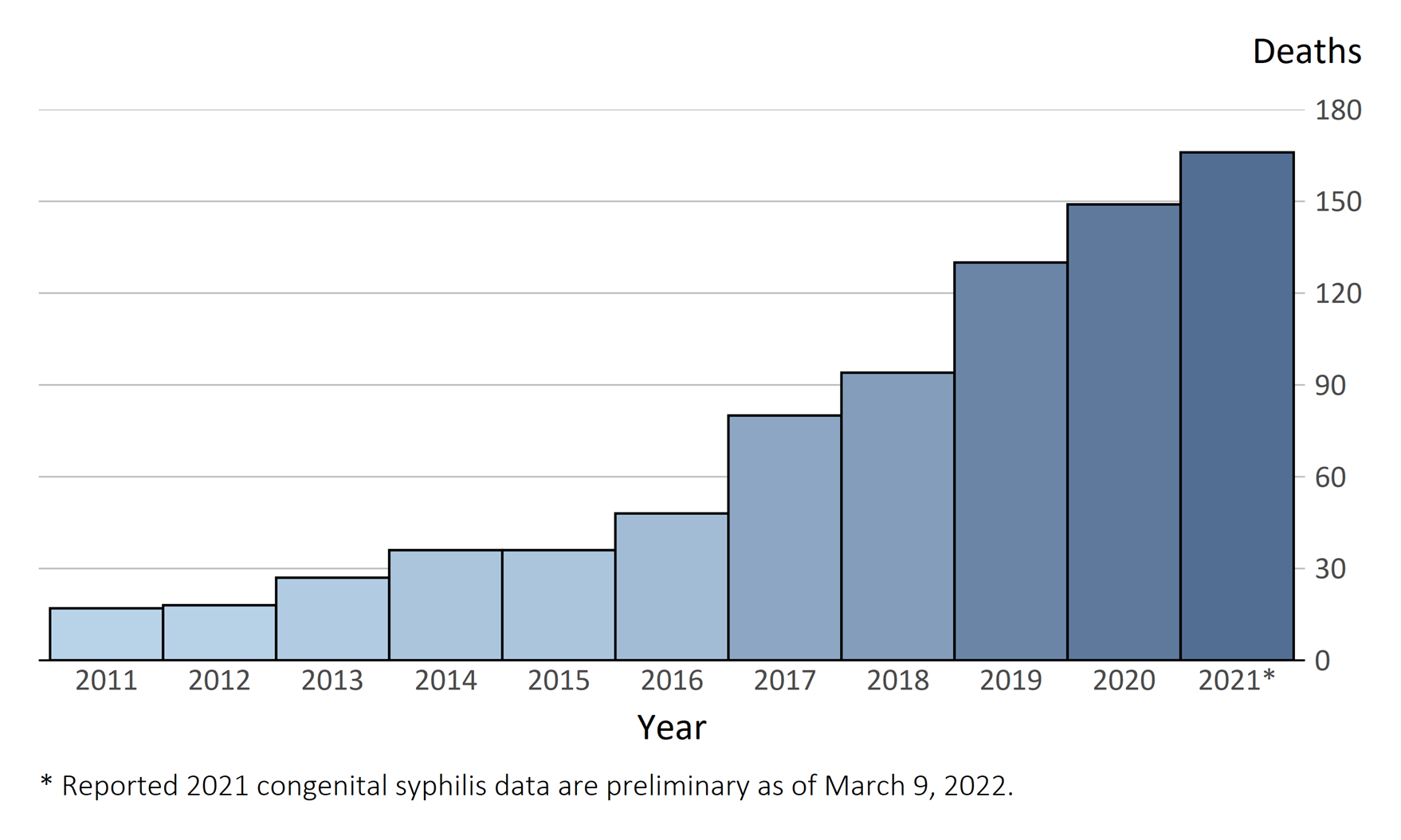
Source: Reference 3 (CDC: Preliminary 2021 Data: Syphilis)
References:
- Pagaoa M, Grey J, Torrone E, Kreisel K, Stenger M, Weinstock H. Trends in nationally notifiable sexually transmitted disease case reports during the US COVID-19 pandemic, January to December 2020. Sex Transm Dis. 2021;48(10):798-804.
- Accessed on April 18, 2022. https://www.cdc.gov/std/statistics/2020/impact.htm
- Accessed on April 18, 2022. https://www.cdc.gov/std/statistics/2020/preliminary2021.htm
- Davidson KW, Barry MJ, Mangione CM, et al; The US Preventive Services Task Force (USPSTF). Screening for chlamydia and gonorrhea: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(10):949-956.
- Bibbins-Domingo K, Grossman DC, Curry SJ, et al; The US Preventive Services Task Force (USPSTF). Screening for syphilis infection in nonpregnant adults and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(21):2321-2327. doi:10.1001/jama.2016.5824
- Thornton C, Chaisson LH, Bleasdale SC. Characteristics of pregnant women with syphilis and factors associated with congenital syphilis at a Chicago hospital. Open Forum Infect Dis. 2022;9(5):ofac169. doi:https://doi.org/10.1093/ofid/ofac169
- Liddon N, Pampati S, Dunville R, Kilmer G, Steiner RJ. Annual STI testing among sexually active adolescents. Pediatrics. 2022;149(5):e2021051893.

