Outbreaks, Alerts and Hot Topics
February 2021
COVID-19 Transmission in Schools

Angela Myers, MD, MPH | Director, Division of Infectious Diseases | Professor of Pediatrics, UMKC School of Medicine | Medical Editor, The Link Newsletter
We are now well into the third quarter of the school year, and I, along with many others, are hopeful that our next school year will be different than this one has been, and that in-person learning will be the norm. There are several recent publications showing that in-person school works well if the correct mitigation strategies are employed. This gives me hope that someday, in the not-too-distant future, I will have two teenagers who are in school full time.
Seventeen K-12 schools in rural Wisconsin opened to in-person learning and implemented several safety measures including masks, small cohorts of students (11-20 per group), physical distancing of 6 feet whenever possible, and quarantining those who were exposed to COVID-19. A study of the schools included nearly 5,000 students and 650 staff members. Rates of COVID-19 infection attributed to school spread were compared to infection rates in the community.1
Community positivity rates varied from 7-40% of those tested. Masking was required and reported by teachers filling out a weekly study survey. Mask-wearing was reported to occur in ~95% (92-97%) of students. COVID-19 case rates were lower for students and staff members (3,453:100,000) compared to the community rate in the county (5,466:100,000). There were 191 cases in all; 133 in students and 58 in staff members during the study period, and all cases were investigated by contact tracers to determine school of community spread.
Based on contact tracing, seven (3.7%) cases among students were found to be related to school transmission. However, no staff cases were found to be acquired at school. In other words, all the staff cases were related to community transmission. There was no student transmission between different student cohorts, and the incidence of COVID-19 in schools during this study was 37% lower than community transmission.
Data from the North Carolina ABC Science Collaborative (ABCs) is similar to the Wisconsin data. This study was conducted over the first quarter of the school year and included 11 school districts with 100,000 students and staff.2 Schools tracked initial and secondary cases, which were also adjudicated by the local health department.
During the first nine weeks of the school year, there were 773 cases of community-acquired COVID-19. Thirty-two additional cases were identified by contact tracing to have been acquired within schools. Of these 32 secondary transmission cases, six occurred in pre-K, 11 in elementary, six in middle, five in high schools, and four in K-12 schools. Most occurred due to absent face coverings in young children, while eating lunch, or among children with special needs who could not safely mask.
They did not find any student-to-staff transmission within the schools. The ABC group cited several factors that contributed to the success of their partnership with the school districts. First, there was a focus on the “3Ws" (i.e., wear a mask, wait 6 feet, and wash hands)” across all the schools. Second, the superintendents met regularly to share best practices and lessons learned. Finally, the school districts worked closely with the health department to report all infections and perform contact tracing.
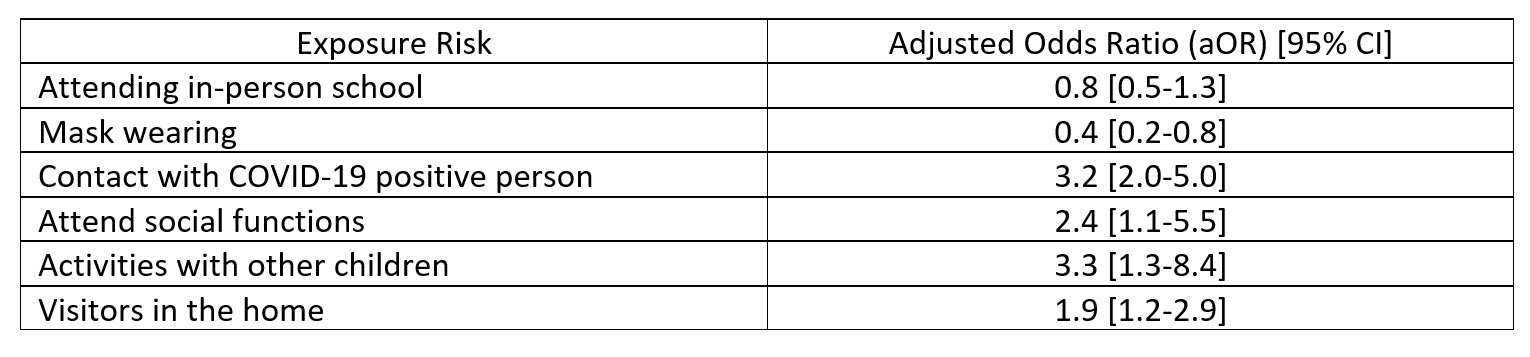
The Mississippi health department worked with the CDC to perform a case-control study of 397 (154 cases; 243 controls) children <18 years of age who were tested for COVID-19. Parents were interviewed about their child’s exposures, and those who tested positive for COVID-19 were compared to those who tested negative.3 The risk factors identified for COVID-19 positive cases included exposure to someone with known COVID-19, attending gatherings with people other than from their household, having visitors in the home, or participating in activities with other children (e.g., birthday parties). Wearing masks appeared to mitigate risk, and attending school was not found to be a risk factor for COVID-19 infection. Table 1.
Finally, Scientists from the CDC published a viewpoint article in JAMA recently outlining necessary measures for in-person school. Their recommendations include implementing prevention strategies that mitigate community transmission such as indoor dining restrictions, avoiding indoor practices without distancing, and sports tournaments when community transmission is high.4
Table 1. Factors mitigating and increasing risk of COVID-19 infection among school-aged children.
References:
- Falk A, Benda A, Falk P, Steffen S, Wallace Z, Høeg TB. COVID-19 Cases and Transmission in 17 K–12 Schools — Wood County, Wisconsin, Aug. 31–Nov. 29, 2020. MMWR Morb Mortal Wkly Rep. ePub: 26 Jan. 2021. DOI: http://dx.doi.org/10.15585/mmwr.mm7004e3.
- Zimmerman KO, Akinboyo IC, Brookhart A, et al. Incidence and Secondary Transmission of SARS-CoV-2 Infections in Schools. Pediatrics. 2021; doi: 10.1542/peds.2020-048090.
- Hobbs CV, Martin LM, Kim SS, et al. Factors Associated with Positive SARS-CoV-2 Test Results in Outpatient Health Facilities and Emergency Departments Among Children and Adolescents Aged <18 Years-Mississippi, September-November 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1925-29.
- Honein MA, Barrios LC, Brooks JT. Data and Policy to Guide Opening Schools Safely to Limit the Spread of SARS-CoV-2 Infection. JAMA. Published online Jan. 26, 2021. doi:10.1001/jama.2021.0374 https://jamanetwork.com/journals/jama/fullarticle/2775875.
