Evidence-Based Strategies for Common Clinical Questions
August 2021
Protecting Children from Tobacco Smoke Exposure
Author: Abbey Masonbrink, MD, MPH | Pediatric Hospitalist | Clinical Assistant Professor of Pediatrics, UMKC School of Medicine
Column Editor: Kathleen Berg, MD | Co-Director, Office of Evidence-Based Practice | Pediatric Hospitalist, Division of Pediatric Hospital Medicine | Clinical Assistant Professor of Pediatrics, UMKC School of Medicine
While there is no safe level of tobacco smoke exposure, more than half of children in the United States are exposed to tobacco smoke.1,2 Smoke exposure includes second-hand smoke, which is emitted directly from a tobacco product, and third-hand smoke, which is smoke absorbed onto surfaces and then exposed via direct contact or inhalation, causing serious adverse health outcomes in children. Tobacco products include traditional cigarettes, cigars, pipes, hookahs, as well as the newer electronic nicotine delivery systems such as e-cigarettes, e-cigars, e-hookah, and a wide variety of vaping devices (See The Link Volume 13 Issue 7 for recent article, “The Implications of Vaping and Preparedness Post-Pandemic” for details on electronic delivery systems).
Tobacco smoke exposure is linked with increased prevalence of prematurity, sudden infant death syndrome, respiratory diseases (e.g., asthma, bronchiolitis), otitis media, cancer, cardiovascular disease and early mortality.1,3 Also, parental tobacco dependence increases risk for tobacco initiation and dependence among their children.1,4 Pediatricians play an important role in preventing smoke exposure among children by screening for and addressing tobacco smoke exposure during all clinical visits.2,3
Because tobacco cessation counseling is more effective if provided by a physician, evidence-based guidelines recommend that pediatricians inquire about tobacco use and smoke exposure during health supervision visits, as well as visits for diseases that may be exacerbated by smoke exposure. The Clinical Effort Against Secondhand Smoke Exposure (CEASE) program has developed a practical tool (Ask, Assist, Refer) for pediatricians to address parental tobacco use and dependence (See Figure 1 for details).5–7 Pediatricians can ask these two questions to screen for smoke exposure:
- Does your child live with anyone who uses tobacco products?
- Does anyone who provides care for your child smoke?
If there is a positive response to either of these questions, seek more information about who smokes and where the exposure occurs. Pediatricians can then assist the parent or caregiver by offering quit program or smoke-free home resources and provide referral to quit programs (1 (800) QUIT-NOW or Text QUIT to 47848). See http://www.ceasetobacco.org for more details.5 Additionally, Missouri and Kansas both offer smoking cessation support programs.
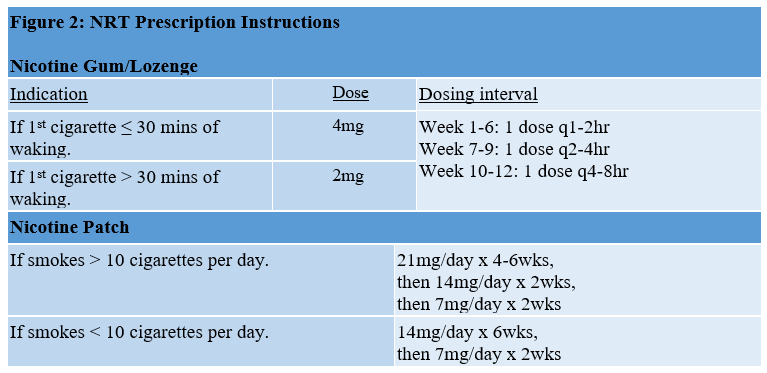
Counseling combined with nicotine replacement therapy (NRT) dramatically improves successful quit rates.2,3 NRT is useful to help control symptoms of nicotine withdrawal and cravings. While this medication can be obtained over-the-counter, as most health insurance partially or fully covers NRT with a physician prescription, pediatricians can assist parents to quit smoking by prescribing NRT. When prescribing NRT, it is important to discuss the benefits and drawbacks of the medications, screen for contraindications, and instruct the caregiver or parent on how to use the product appropriately. Contraindications to NRT include recent (≤ 2 weeks) myocardial infarction, serious underlying arrhythmias, serious or worsening angina pectoris, pregnancy and breastfeeding. Typical combination NRT regimens include use of a daily transdermal patch, roughly equivalent to the total daily cigarette use, to provide a steady dose of nicotine, and as-needed dosing of nicotine gum or lozenge for cravings (See Figure 2 for NRT prescribing instructions). The daily dose of nicotine is then slowly weaned over 10 to 12 weeks.
Pediatricians play an important role in the prevention of tobacco smoke exposure and the numerous related poor health outcomes among children.2,3 Clinicians can utilize each clinical visit to provide this important evidence-based care by screening for tobacco smoke exposure and provide anticipatory guidance to prevent and reduce tobacco smoke exposure. By offering these important services, pediatricians can dramatically impact the short- and long-term health outcomes of their patients and their families.
Figure 1
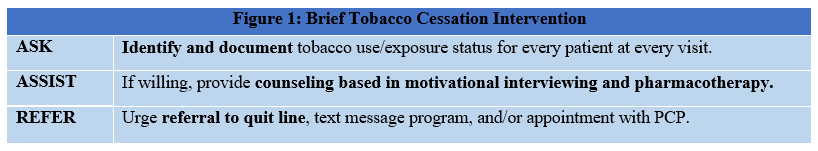
Figure 2
References:
- US Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006.
- Farber HJ, Walley SC, Groner JA, Nelson KE, Section on Tobacco Control. Clinical practice policy to protect children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):1008-1017. doi:10.1542/peds.2015-3108.
- Farber HJ, Groner J, Walley S, Nelson K, Section on Tobacco Control. Protecting children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):e1439-1467. doi:10.1542/peds.2015-3110.
- Vuolo M, Staff J. Parent and child cigarette use: a longitudinal, multigenerational study. Pediatrics. 2013;132(3):e568-577. doi:10.1542/peds.2013-0067.
- Winickoff JP, Hipple B, Drehmer J, et al. The Clinical Effort Against Secondhand Smoke Exposure (CEASE) intervention: a decade of lessons learned. J Clin Outcomes Manag. 2012;19(9):414-419.
- Nabi-Burza E, Drehmer JE, Hipple Walters B, et al. Treating parents for tobacco use in the pediatric setting: the clinical effort against secondhand smoke exposure cluster randomized clinical trial. JAMA Pediatr. 2019;173(10):931-939. doi:10.1001/jamapediatrics.2019.2639.
- Pbert L, Farber H, Horn K, et al. State-of-the-art office-based interventions to eliminate youth tobacco use: the past decade. Pediatrics. 2015;135(4):734-747. doi:10.1542/peds.2014-2037.


