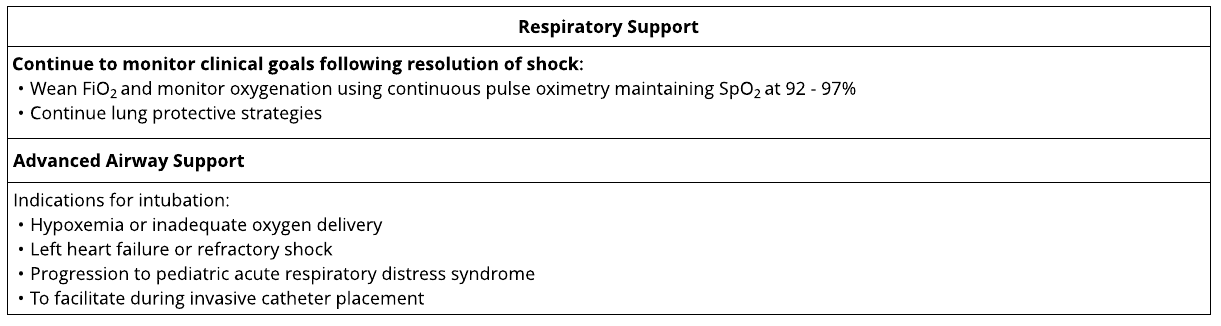
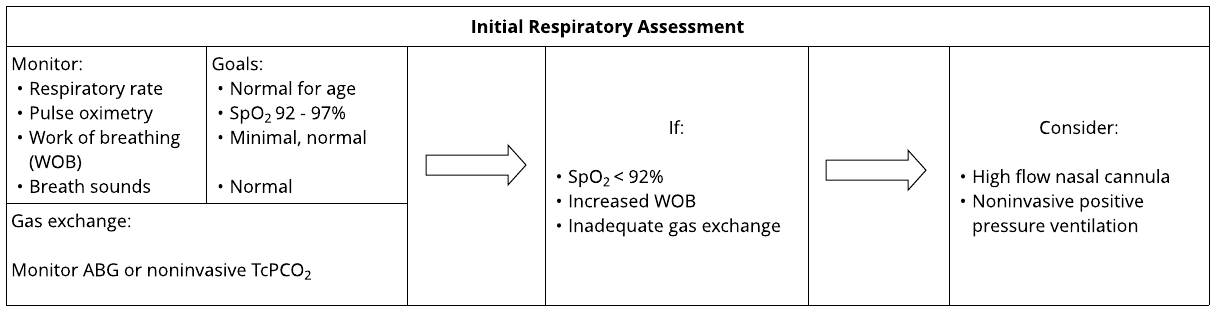
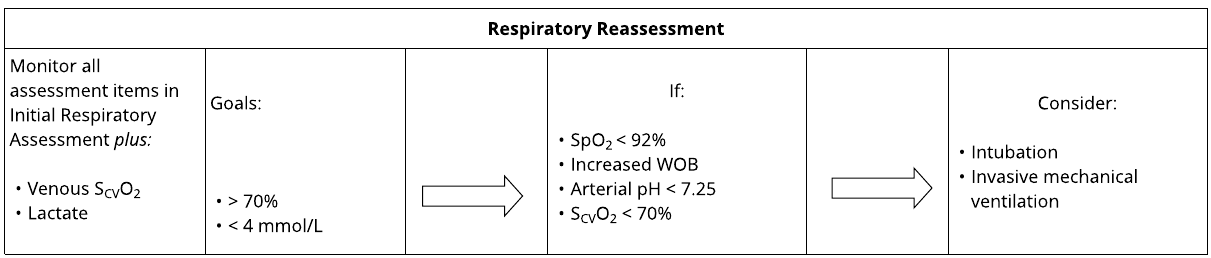
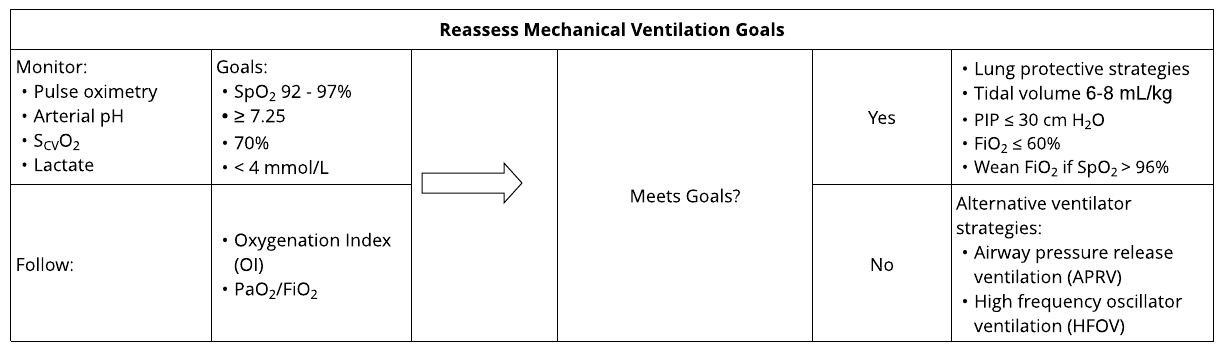
Respiratory Support
These pathways do not establish a standard of care to be followed in every case. It is recognized that each case is different, and those individuals involved in providing health care are expected to use their judgment in determining what is in the best interests of the patient based on the circumstances existing at the time. It is impossible to anticipate all possible situations that may exist and to prepare a pathway for each. Accordingly, these pathways should guide care with the understanding that departures from them may be required at times.