14. Asthma Management in the PICU
The definition of status asthmaticus can vary but is primarily defined by an extreme asthma exacerbation that is non-responsive to initial bronchodilator therapy with hypoxemia, hypercarbia, subsequent respiratory failure and need for mechanical ventilation for support. Children in status asthmaticus have the highest need for support from our pediatric intensive care unit (PICU).
As per our clinical practice guidelines, the following criteria summarizes when a patient should be considered for the PICU.
- Prolonged continuous albuterol for >4 hrs with worsening symptoms
- Inadequate ventilation with hypercapneahypercapnia (PCO2 on capillary blood gas >45)
- Need for high flow nasal cannula or non-invasive ventilation
- Persistent hypoxemia (SpO2 <90%) on supplemental O2 (>2 L/min or >50% FiO2 with non-rebreather)
- Altered level of consciousness (drowsiness, seizures, syncope)
In scenarios where patients are on continuous albuterol for >4 hours in the emergency department or medical/surgical floors, but are improving clinically, clinical status and concerns should be discussed with the accepting location. Signs of improvement include but are not limited to: decreased respiratory rate, decreased oxygen requirement, decreased respiratory care score, or decreased pediatric early warning score (PEWS). Other relevant considerations include whether or not a patient’s respiratory demands exceed staffing ratios allotted on inpatient medical floor.
Consideration for need to increase to higher level of care should be considered if there is concern for impending or actual respiratory arrest. The progression from respiratory distress to respiratory failure to respiratory arrest can vary by patient. Respiratory failure can progress rapidly and be difficult to reverse. Therefore, it is important to emphasize the signs of impending respiratory arrest.1
- Altered level of consciousness (LOC): this may manifest as drowsiness or sleepiness in young children. Hypoxemic seizures or syncope can also be a complication to status asthmaticus.
- No improvement after magnesium sulfate administration in conjunction with continuous albuterol.
- If available, a Pediatric Early Warning Systems (PEWS) score of 6 or Respiratory Care Score greater than 9 without improvement.
- Oxygen requirement greater than 50%.
- Hypoventilation: this may develop more rapidly in young children.
- Hypercapnia: Monitoring carbon dioxide levels is a useful indicator of impending failure. Arterial blood gas with PCO2 >42 is associated with high risk of impending respiratory arrest in acute situations.
- Paradoxical thoracoabdominal movement, “Seesaw breathing”
- Absence of wheezing: airway obstruction is so severe that no air can be auscultated. This can be especially difficult to detect for novice health care providers; hence, auscultatory findings should be considered in clinical context.
- Bradycardia: heart rate changing from tachycardia to bradycardia
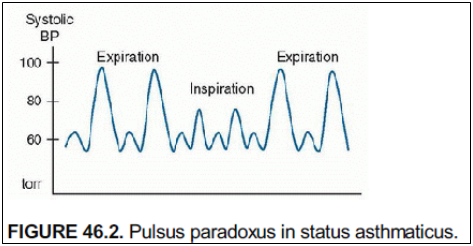
- Resolution of prior pulsus paradoxus – in the absence of improving respiratory status, resolution of pulsus paradoxus suggest respiratory muscle fatigue.
Basic pathophysiology of asthma exacerbation
Lower airway obstruction due to:
- Bronchial smooth muscle contraction (“bronchoconstriction”)
- Increased mucous production leading to mucous plugging
- Airway inflammation and edema
Cardiopulmonary interactions in asthma exacerbation
- Hyperinflation of lungs leads to increased pulmonary vascular resistance. This then leads to increased right ventricle afterload with subsequent decreased right ventricular function.
- High intrathoracic pressure from hyperexpanded lungs leads to decreased preload to the heart, thereby decreasing cardiac output.
Evaluation
History
Important history talking points:
- Asthma severity
- Medication adherence
- Previous ED/Urgent Care visits or oral steroid courses
- Previous hospitalizations
- Previous ICU admissions
- Previous need for intubation and mechanical ventilation extracorporeal membrane oxygenation (ECMO)
- Triggers, specifically for this admission
- Signs/symptoms of concomitant viral or bacterial infection
Physical Examination
- Vitals: Respiratory rate and oxygen saturation is the minimum requirement; but, a full set of vital signs is important to assess patient's status.
- Albuterol can cause temporary V/Q mismatching resulting in mild hypoxemia
- Albuterol can cause temporary V/Q mismatching resulting in mild hypoxemia
Pulsus paradoxus (large negative intrathoracic pressure during inspiration leads to increased left ventricle afterload which manifests as decreased systolic blood pressure.
- Auscultation: Typically, children will have prolonged expiratory phase. Wheezing can be inspiratory, expiratory or both (biphasic) but is from the lower airway and classically polyphonic noise.
- Quality of air movement – lack of wheezing combined with poor air movement is very concerning!
- Quality of air movement – lack of wheezing combined with poor air movement is very concerning!
- Work of Breathing:
- Evaluate for typical signs of respiratory distress – retractions, grunting, nasal flaring, head bobbing.
- Distress may be more subtle in older children/teens or in patients with a history of severe baseline obstructive lung disease.
- Can they speak in complete sentences? Or only three-word phrases? One word at a time?
- Evaluate for typical signs of respiratory distress – retractions, grunting, nasal flaring, head bobbing.
Imaging & Laboratory Evaluation
- Chest X-ray:
- Often hyperinflated with flattened diaphragms due to air trapping
- Narrow cardiac silhouette due to high intrathoracic pressure
- Evaluate for signs of viral or bacterial infection
- Look for subcutaneous air, /pneumomediastinum, pneumothorax.
- Often hyperinflated with flattened diaphragms due to air trapping
- Laboratory Evaluation: blood gas, complete blood count with differential, consider infectious work up if necessary for isolation placement or if it may change management.
Treatment Options
(Available in Powerplan “PICU Status Asthmaticus”)
An outline of pharmaceutical options in the PICU is briefly reviewed below. For further information on other pharmaceutical therapies, please see asthma medications.
Continuous albuterol
- Dosed at 5, 10, 15 or 20 mg/hr. Can be administered via simple face mask, HFNC, or non-invasive ventilation.
- Mechanism: beta 2 receptor agonist leading to airway smooth muscle
- Side effects: tachycardia (via beta 1 agonism), agitation/hyperactivity, tremors, dysrhythmias, hyperglycemia, hypokalemia, diastolic hypotension with subsequent ECG changes, elevated troponin levels have been described.
- CMH caveat: Nebulized bronchodilator solutions in the United States can include preservative products that cause bronchospasm. These preservative products are sulfites, benzalkonium chloride (BAC), and chlorobutanol. In particular, BAC can lead to bronchoconstriction; this bronchoconstriction is cumulative, prolonged, and correlates with airway hyperresponsiveness. At CMH, we do not use BAC containing products, but these can be used at outside institutions and contribute to unresponsive bronchoconstriction.
IV corticosteroids
- All asthma patients admitted to PICU should receive IV corticosteroids.
- Mechanism: suppress cytokine production and inflammation
- Typically, this is IV Solumedrol (methylprednisolone). High glucocorticoid effect and minimal mineralocorticoid effect
- Dose is 2 mg/kg load followed by 0.5-1 mg/kg q6hr.
- Side effects: hyperglycemia, hypertension, agitation
IV Magnesium sulfate
- Mechanism: smooth muscle relaxation
- Dose is 25-50 mg/kg IV over 30-60 minutes or drip at 10-20 mg/kg/hr
- Often given in conjunction with a small fluid bolus as it can cause hypotension.
- Side effects: hypotension, central nervous system depression, flushing.
Ipratropium bromide (Atrovent)
- Mechanism: anticholinergic that impairs bronchial smooth muscle contraction
- Dose is 125-500 mcg neb or 4-8 puffs q4-8 hours
- Can also be delivered in a combination medication for nebulization; Ipratropium + albuterol = “DuoNeb®” (3 mg of albuterol sulfate and 0.5 mg of ipratropium bromide).
- CMH caveat: There is no combined DuoNeb® respule; albuterol and ipratropium are ordered separately and the respiratory therapist will combine during treatment.
- Side effects: dry mouth, flushing, tachycardia
Subcutaneous or intramuscular Epinephrine
- Can be given in Emergency Department or en route to PICU when air movement is so poor that inhaled bronchodilators are ineffective.
- Mechanism: stimulates all adrenergic receptors (alpha, beta1, beta2). For asthma, beta 2 agonism leads to bronchodilation.
- Dose is 0.01 mg/kg up to max of 0.5 mg. May be repeated 1-2 times every 20 minutes
- Practical Pearl: Most home epinephrine pens are dosed at 0.15 mg for 15-30 kg patient or 0.3 mg for >30 kg pt.
- Practical Pearl: Most home epinephrine pens are dosed at 0.15 mg for 15-30 kg patient or 0.3 mg for >30 kg pt.
- Risks: lack of control over dose especially if using a standardized epinephrine pen, difficult to “down-titrate” for complications
- Side effects: arrhythmia, cardiomyopathy, glucose changes, hypokalemia, tissue necrosis at site, jitteriness/shakiness, headache, nausea, excessive doses can cause constriction of skeletal and vascular smooth muscle.
Terbutaline
- Intravenous formulation makes it useful if air movement is so poor that inhaled bronchodilators are not effective.
- Beta 2 receptor agonists lead to bronchial smooth muscle relaxation, with less effect on heart rate.
- Dosing: IV: 10 mcg/kg load then drip at 0.1-10 mcg/kg/min; Sub-Q: 0.01 mg/kg/dose q 15-20 min x3
- Side effects: tachycardia, dysrhythmias, nervousness, decreased serum potassium, increased serum glucose, tremor.
Aminophylline
- Mechanism: methylxanthine derivative. Non-selective phosphodiesterase (PDE) inhibition leading to bronchodilation, inflammatory downregulation
- Dose 5-7 mg/kg load, then drip at 0.5-0.9 mg/kg/hr
- Serum concentrations must be checked. Goal level 10-20 (very narrow therapeutic window)
- Side effects: nausea/vomiting, tachycardia, irritability. Seizures or arrhythmia can occur with high levels (>35)
- Used less commonly at CMH.
Ketamine
- Mechanism: bronchodilation via multiple potential mechanisms - immunomodulation, catecholamine upregulation, decreased nitric oxide, anticholinergic effects
- Dose as continuous drip at 0.5-1 mg/kg/hr
- Often used for sedation when intubating an asthmatic, dose is 1-2 mg/kg.
- Side effects: tachycardia, hypertension, hallucinations, increased secretions, laryngospasm
Respiratory Support in ICU
An outline of respiratory support modalities is provided here. For further discussion, please also see section on Respiratory Support for Asthma Exacerbation.
Respiratory support in the ICU can range from nasal cannula to mechanical ventilation. Respiratory support that can only be given in the ICU includes Non-Invasive Ventilation (e.g., continuous positive airway pressure or bilevel positive airway pressure), invasive ventilation or extracorporeal membrane oxygenation (ECMO).
- CMH Caveat: Children 4 weeks to 24 months of age with viral bronchiolitis may be allowed to use HFNC (2 L/min/kg up to 15 L/min with FiO2 max of 40%) on inpatient floors. Please discuss with attending and RT.
Heliox
- Mixture of helium and oxygen gas with a density less than room air.
- Mechanism: improves laminar flow, may improve distribution and deposition of nebulized medications. This leads to decreased work of breathing for disorders characterized by airways resistance (e.g. asthma, COPD, BPD, upper airway obstruction).
- Tanks are available in 80:20 (80% helium 20% oxygen mixture).
- If patients need increased FiO2, this can be bled into the system and decreased ratio of helium to oxygen.
- There is controversy regarding use in acute asthma exacerbations with some studies finding benefit and others that found none.
- Heliox does NOT replace bronchodilation and corticosteroid therapy and should only be considered as adjunctive care.
- Can only be delivered in ED or PICU.
Inhaled anesthetics (isoflurane, sevoflurane)
- Administered only by anesthesia in rooms with scavenger system and specialized ventilator (e.g., operating room)
- Administered in intubated/mechanically ventilated patients with life threatening bronchospasm. Mechanism of action: bronchodilation via multiple mechanisms
- Side effects: sedation, hypotension, dysrhythmia
- Risks of use in PICU without a scavenger system includes difficulty monitoring, volatility of gas, and impact on health care providers.
Mechanical ventilation in Status Asthmaticus
- Indications
- Respiratory failure with profound hypercarbia/acidosis
- Decreased mental status
- Severe refractory hypoxia
- Respiratory failure with profound hypercarbia/acidosis
- There is a high risk for cardiac arrest during intubation
- High intrathoracic pressure leads to decreased preload with subsequent decreased cardiac output and hypotension.
- Anticipate hypotension and give volume!
- High intrathoracic pressure leads to decreased preload with subsequent decreased cardiac output and hypotension.
- Risks of mechanical ventilation in status asthmaticus include:
- Worsening bronchospasm
- Ventilator induced lung injury, especially barotrauma and volutrauma
- Air leak, pneumothorax, pneumomediastinum
- Hypotension due to decreased preload
- Infection
- Worsening bronchospasm
Ventilator management
- Typically want low rate with long expiratory time (I:E of 1:4 or 1:5)
- Low tidal volume (5-6 mL/kg), low peak pressures
- Permissive hypercapnea
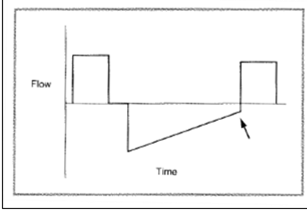
- Watch for auto-peep (alveolar air trapping)
- Make sure measured PEEP (total PEEP) is not higher than set PEEP by performing an expiratory hold (Total PEEP – set PEEP = Auto PEEP).
- Avoid paralysis
Ventilator wave forms in status asthmaticus:
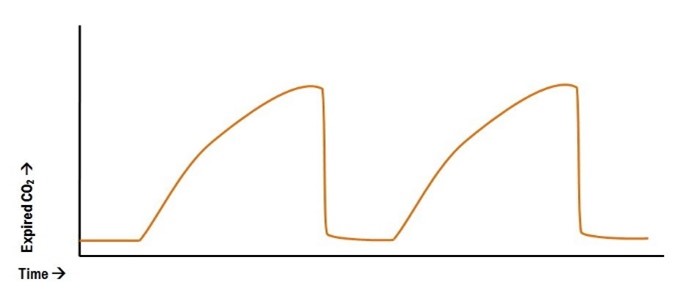
May see “ramping” of end tidal due to bronchospasm on end tidal CO2 trends An example is below:
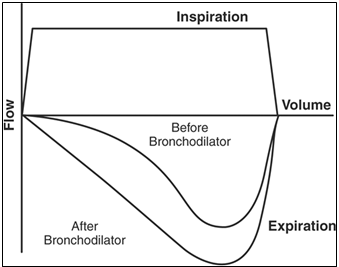
Flow patterns on ventilator can also show scooping on expiratory limb with improvements after bronchodilator.
Flow patterns on a ventilator may also show air trapping as the expiratory flow limb does not return to baseline indicating ongoing air trapping.
Extracorporeal Membrane Oxygenation (ECMO)
A full discussion on ECMO is outside the scope of this reference guide. Brief indications for ECMO include:
- Worsening hypoxemia despite maximal support or mechanical ventilation
- Worsening air leak
- Worsening acidosis (respiratory or metabolic)
It is important to continue asthma management, i.e. steroids, albuterol, etc. while on ECMO. Consideration for extubating while on ECMO can also be made once patient is stable.
Transfer out of PICU
Patients who are admitted for severe asthma exacerbation to the PICU fulfill the High-Risk Asthma Program (HRAP) criteria. Please use the high-risk power plan.
Consultation to Pulmonary Medicine should be done if patient has been seen in outpatient Pulmonary clinic in the past 2 years. Please place a consultation to Allergy & Immunology Medicine if patient has been seen in the past 2 years. If patient has been seen by neither subspecialty team, consultation for follow up asthma care is per PICU attending preference.
For patients with food allergy along with asthma, we suggest consultation to Allergy/Immunology for comprehensive management of asthma and food allergy.
Recommended reading
Fuhrman & Zimmerman’s Pediatric Critical Care, 5th Ed. Chapter 53: Asthma.
- NAEP - EPR3 2007. Guidelines for the diagnosis and management of asthma. Bethesda MD: US dept of Health and Human Services, NIH
- Asthma Reference Guide Home
- 1. Introduction to Asthma
- 2. Asthma Diagnosis
- 3. Asthma Presentation
- 4. Goals of Asthma Therapy and Management
- 5. Asthma Severity and Asthma Control
- 6. Asthma Outpatient Management
- 7. Treating Modifiable Risk Factors
- 8. Treating Co-Morbid Conditions
- 9. Asthma Medications
- 10. Yellow Zone Therapy Options
- 11. Allergy Immunotherapy and Biologic Therapy
- 12. Asthma Exacerbations in the Emergency Department or Urgent Care
- 13. Special Asthma Considerations for Inpatient
- 14. Asthma Management in the PICU
- 15. Respiratory Support for Asthma Exacerbation
- 16. Asthma Education Resources
