Clinical Experience
Pediatric Critical Care Medicine Fellowship
Clinical rotations occur in four-week blocks. All call is in-house with a critical care attending. First-year fellows typically have six calls per block; second- and third-year fellows have five calls per month during their scholarly blocks and three calls per month during their clinical blocks.
Total Clinical Weeks 84 weeks
Total Research/Vacation Weeks 72 weeks
|
Year |
PICU Weeks |
Other Clinical Weeks |
Research Weeks |
Total Weeks |
|---|---|---|---|---|
|
I |
28 |
14 |
10 |
52 |
|
II |
20 |
0 |
32 |
52 |
|
III |
20 |
2 |
30 |
52 |
Competency-based objectives for the rotations are available: first year, second year, third year.
2-Year Fellowship (For fellows who have previously completed a pediatric cardiology fellowship)
|
Year |
PICU Weeks |
Other Clinical Weeks |
Research Weeks |
Total Weeks |
|---|---|---|---|---|
|
I |
28 |
8 |
16 |
52 |
|
II |
30 |
4 |
18 |
52 |
|
III |
30 |
4 |
18 |
52 |
Pediatric Intensive Care Unit (PICU)

Our 43-bed Pediatric Intensive Care Unit and 24 bed Cardiac Intensive Care Unit have over 2300 admissions per year. Since 1997, the pediatric critical care faculty has provided 24-hour in-house coverage. The ECMO program in the pediatric intensive care unit was initiated in 2007 with 40-50 cases and 500-600 patient days annually, utilizing both VV and VA modalities.
We have a busy trauma surgery service with the only Level-1 Trauma center in a free standing children’s hospital in our geographic area. We are working towards becoming an American Burn Association certified center. We have active liver, kidney, and bone marrow transplant programs. We have an active congenital heart disease program and pediatric cardiac transplant program that includes a VAD program with more than 350 cardiovascular surgeries per year. We have incorporated advanced practice nurses into the cardiac care team, and advanced practice nurses and intensive care hospitalists into the medical team.
Anesthesia
Fellows will rotate in the department of anesthesiology for two months during the first year of training. Advanced airway skills, vascular access and the physiologic response to general anesthetics are emphasized. During the second month, fellows will spend time in the cardiovascular operating room, becoming familiar with the anesthetic nuances of children with congenital heart disease and gaining exposure to cardiopulmonary bypass. Third-year fellows may spend an additional two weeks learning the skills of procedural sedation outside of the pediatric intensive care unit.
Cardiology
First-year fellows will spend two weeks focused on the care of children with congenital and acquired heart disease. The rotation includes exposure to the cardiac catheterization lab; interpretation of cardiac waveforms; basic echocardiogram interpretation; arrhythmia classification and treatment; and surgical correction or palliation.
Transport
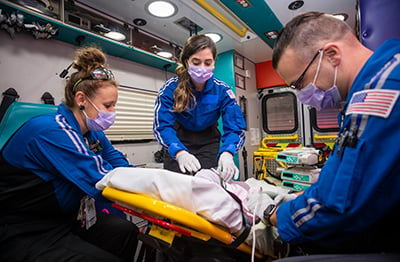
Fellows participate in a four-week rotation during their first year with the transport team, participating in local and regional transports by ground transport, rotor wing and fixed wing aircraft. The in-house transport team, comprised of an advance clinical nurse and respiratory therapist serves a 150-mile radius and transports more than 5700 patients per year with medical direction provided by the intensivist.
During the third year of training, fellows will gain experience communicating with referring physicians and guiding the transport team in the care of the children we transport.
Children's Mercy Critical Care Transport in Kansas City, Mo. is a 24-hour a day dedicated pediatric- and neonatal-critical care transport program, and winner of the Transport Program of the Year, sponsored by the Association of Air Medical Services.
Children's Mercy Critical Care Transport has earned the Fixed Wing Award of Excellence and the Critical Care Ground Award of Excellence.
Specialty opportunities at Children’s Mercy

Have an interest in cardiac ICU as a career? The pediatric critical care fellowship at CM provides the maximum ACGME allowed CICU rotations, 6 blocks over 3 years. We additionally take 6 months of CICU call. Thus you are well positioned for a career in the CICU after the cardiac exposure in our program.
Want to dual board eligible in cardiology and critical care? We have a two-year program we recruit for in even number years for trainees who will successfully complete a cardiology fellowship.
Have a clinical pharmacology interest? We have the only accredited training program in the country. T32 programs are available and would represent a 4th year of training. Learn more by visiting our Pediatric Clinical Pharmacology Fellowship page.
Have a global health interest? We are one of few pediatric critical care programs with access to a global health program. The engagement in this work can vary based on level of interest. Learn more by visiting our Global Health page.
Have a health care administration interest? With administrative positions continually growing, there is a increasing opportunity for physicians in these roles. Learn more about the one additional year fellowship and note the degree eligibility requirements. Visit our Administrative Fellowship page.
Our PICU Fellowship leadership team
Andrew Ausmus, MD
Program Director
(816) 234-3014
aausmus@cmh.edu
Gene Peir, MD
Associate Program Director
(816) 234-3041
ghpeir@cmh.edu
Toni Zaner, BA
Fellowship Coordinator
tmzaner@cmh.edu
