Evidence-Based Strategies for Common Clinical Questions
January 2021
A Brief Review of a Brief Event: An Approach to the Higher-Risk BRUE

Author: Daniel Mulhall, MD | Chief Resident of Pediatrics
Column Editor: Kathleen Berg, MD | Pediatric Hospitalist, Division of Pediatric Hospital Medicine | Clinical Assistant Professor of Pediatrics, UMKC School of Medicine
In 2016, the American Academy of Pediatrics published clinical practice guidelines that not only rebrand Apparent Life-Threatening Event as Brief Resolved Unexplained Event (BRUE), but also stratify patients as higher or lower risk and provide a summary of the evidence-based recommendations for those patients whose events meet lower-risk criteria for a serious underlying disorder.1
Patients considered lower-risk are those who are > 60 days in age and > 32 weeks gestational age who present for a single BRUE that lasted < 1 minute in duration and did not require cardiopulmonary resuscitation (CPR) by a trained provider. Exclusion criteria for lower-risk additionally include those who have concerning physical examination findings, such as signs of external injury (e.g., bruising, abrasion, torn frenulum), and those who have a family history of sudden death. The guidelines for lower-risk patients emphasize education of families on BRUEs, provision of resources including CPR training, and employment of shared decision-making with families. Multicenter studies have demonstrated that additional testing most often leads to increased family anxiety without revealing an underlying diagnosis.2,3 Since release of the clinical practice guidelines, admission rates for lower-risk BRUE have decreased by 18%, with significantly lower rates of additional laboratory testing and imaging.4 However, a similar clinical practice guideline does not yet exist for those who are considered higher-risk. Instead, a tiered evaluation is recommended.
Patients with higher-risk BRUE events (Table 1) require prompt evaluation to identify illnesses that could lead to serious adverse outcomes if not addressed quickly. Additionally, patients should be evaluated for common disease processes in which timely intervention could prevent similar events from recurring. For patients identified as having experienced a higher-risk BRUE the following may be considered: at least four hours on continuous pulse oximetry, social work consultation, feeding evaluation, electrocardiogram, blood glucose, venous blood gas, lactic acid and hematocrit, rapid viral respiratory panel and pertussis testing for at-risk patients.5 If there is concern for child maltreatment, evaluation for trauma with neuroimaging and skeletal survey, as well as consultation with experts in child abuse, are recommended.3,5 As BRUE remains a diagnosis of exclusion, if diagnostics reveal an alternative diagnosis, then the patient no longer meets BRUE criteria and should be managed accordingly based on their identified disease process.6
Without an alternative explanation for the higher-risk BRUE, it is recommended that a discussion be conducted with the family regarding benefits and risks of admission to the hospital for observation.5,7 Hospitalization is not strictly required if the family has reliable access to medical care and close follow-up with the primary care clinician is arranged.5 This decision is difficult, however, since current evidence does not reveal which higher-risk patients may benefit from hospitalization. If shared decision-making results in admission, clear communication about the goals of observation are incredibly important, as odds of a repeat event or identification of an underlying condition are low.5,9
Patients admitted to the hospital should be placed on continuous pulse oximetry and closely observed for repeat events for 24 hours. During this time, witnessed events may have specific characteristics prompting further diagnostic work-up for alternative diagnoses such as dysphagia, gastroesophageal reflux disease, central or obstructive apnea, seizures, congenital heart disease or arrhythmia, or fasting metabolic derangements.8 CRP training should be provided to families prior to discharge.5
Primary care clinicians are essential in the evaluation and management of patients with both lower- and higher-risk BRUEs, and may coordinate outpatient evaluation for those families with whom they have an established relationship. With shared decision-making, this strategy has been shown to be an efficient use of community resources while limiting excessive anxiety experienced in a hospital setting.10 BRUEs remain challenging, but with an evidence-based approach, primary and acute care clinicians can use risk stratification to ensure thorough evaluation, while limiting the burden of false positives or over-diagnosis and avoiding hospitalization when appropriate.11 They can provide essential follow-up to determine if further evaluation or referral to subspecialty care is indicated, particularly for recurring events. When additional work-up is not needed, empowering and reassuring families is equally important.
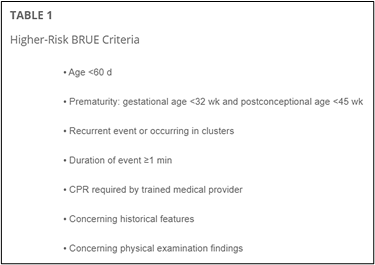
Image from Merritt et al.5 https://pediatrics.aappublications.org/content/144/2/e20184101
References:
- Tieder JS, Bonkowsky JL, Etzel RA, et al. Brief Resolved Unexplained Events (Formerly Apparent Life-threatening Events) and the Evaluation of Lower-Risk Infants. Pediatr. 2016 May;137(5):e20160590.
- Tieder JS, Altman RL, Bonkowsky JL, et al. Management of Apparent Life-threatening Events in Infants: A Systematic Review. J Pediatr. 2013 Jul;163(1):94–9.e1–6.
- Brand DA, Altman RL, Purtill K, Edwards KS. Yield of Diagnostic Testing in Infants Who Have Had an Apparent Life-threatening Event. Pediatr. 2005 Apr;115(4):885–93.
- Ramgopal S, Noorbakhsh KA, Callaway CW, et al. Changes in the Management of Children with Brief Resolved Unexplained Events (BRUEs). Pediatr. 2019 Oct;144(4):e20190375.
- Merritt JL, Quinonez RA, Bonkowsky JL, et al. A Framework for Evaluation of the Higher-Risk Infant after a Brief Resolved Unexplained Event. Pediatr. 2019 Aug;144(2):e20184101.
- Radovanovic T, Spasojevic S, Stojanovic V, Doronjski A. Etiology and Outcome of Severe Apparent Life-threatening Events in Infants. Pediatr Emerg Care. 2018 Oct;34(10):687–90.
- Mittal MK, Sun G, Baren JM. A Clinical Decision Rule to Identify Infants with Apparent Life-threatening Event Who Can be Safely Discharged from the Emergency Department. Pediatr Emerg Care. 2012 Jul;28(7):599–605.
- Kiechl-Kohlendorfer U, Hof D, Peglow UP, Traweger-Ravanelli B, Kiechl S. Epidemiology of Apparent Life-threatening Events. Arch Dis Child. 2005 Mar;90(3):297–300.
- Claudius I and Keens T. Do All Infants with Apparent Life-threatening Events Need to be Admitted? Pediatr. 2007 Apr;119(4):679–83.
- Green M. Vulnerable Child Syndrome and its Variants. Pediatr Rev. 1986 Sep;8(3):75–80.
- Coon ER, Quinonez RA, Moyer VA, Schroeder AR. Overdiagnosis: How Our Compulsion for Diagnosis May be Harming Children. Pediatr. 2014 Nov;134(5):1013–23.

